
Quantitative Percussion Diagnostics: Going Beyond the Human Eye
Today’s dental patients expect to keep their teeth for a lifetime, which means the life expectancy of a tooth has grown from 40–50 years in our grandparents’ time to 90–100 years for our younger patients. Relatedly, scientific studies have also shown that maintaining teeth for a lifetime is associated with better overall physical health.
One of the more difficult diagnostic challenges is finding structural abnormalities early in the destruction process: Fractured teeth, loose crowns, damaged periodontal ligaments, and loosening restorations typically aren’t diagnosed until the problem is severe, often painful, and visually detectable. Many of our traditional tools are qualitative, not quantitative, and conventional visual technologies in dentistry such as radiographs and clinical examinations don’t let us know how a jeopardized tooth responds to loading forces during mastication and parafunction.
Dental implants aren’t impervious to structural failures and disease, either. Yet once an implant has received its final restoration, diagnostic tools intended to help keep implants healthy are limited to the same visual methods used for natural teeth, unless the dentist and patient are willing to remove all restorations down to the implant fixtures and measure via one of several radiofrequency systems available.
QPD: An exacting measurement of percussion
Quantitative percussion diagnostics (QPD) is a practical, instrumented approach to diagnosing structural problems in teeth and final restorations on implants.
QPD was originally used as a research tool to measure the damping mobility of a tooth or implant site; the research version of this technology, the Periometer, was cleared by the Food and Drug Administration in 2008 to measure micromobility of teeth and dental implants. As more of its capabilities were discovered, it was determined that QPD could be beneficial in daily clinical use, providing data that traditional diagnostic aids couldn’t. One great benefit was that dental implants could be restored at any stage of their life — at placement, when deciding to load, at the abutment delivery, even after a final restoration is delivered — without requiring any disassembly.
A clinical version of QPD technology, InnerView by Perimetrics, has recently been introduced to the dental community. The system uses an instrument to apply light percussion to the buccal surface of the tooth or implant, measures the mechanical response, evaluates the data using several algorithms, and provides an evaluation to the operatory almost immediately.
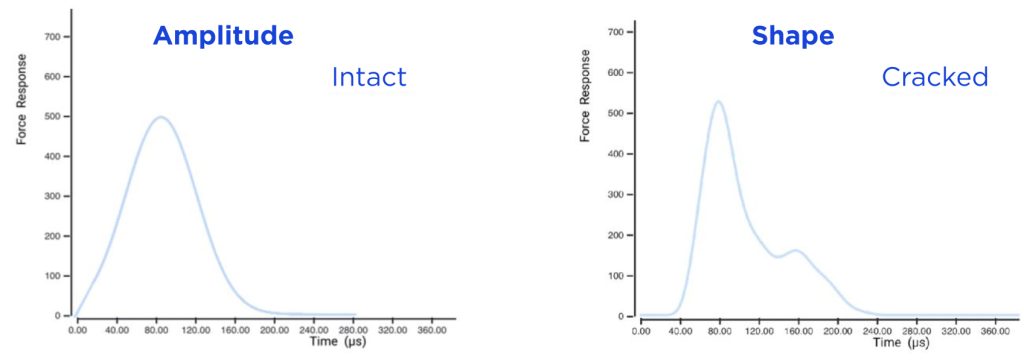
The overall mobility of the entire site, as well as any micromovement in any portion of it, is captured in an energy return graph (ERG), which depicts the mechanical response of the dental site as a function of time. The maximum height of the energy data in this graph characterizes the overall mobility of the structure. A perturbation in the shape of the graph (Figs. 1a and 1b) indicates a microgap defect in the dental structure, such as a crack, loss of cement, or damaged periodontal ligament.
The level of mobility measured by this data is typically not visible to the human eye, but it directly indicates the structural stability of the site, such as the level and quality of osseointegration of an implant. The more micromobility in a site, the weaker the osseous bond, even if the radiograph looks perfect.
Examples of InnerView technology in use
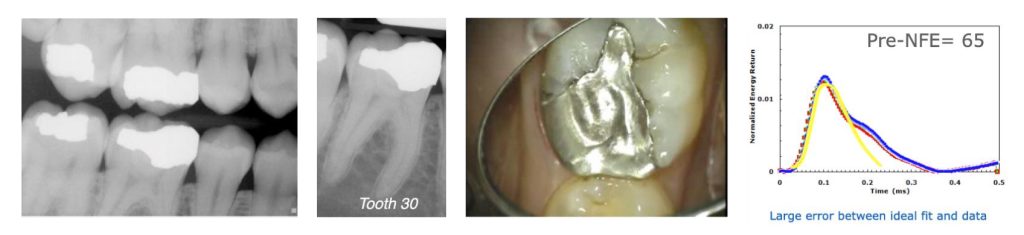
Case 1: Leaking restoration and tooth fracture
Tooth #30 in a 22-year-old woman was slightly sensitive to cold. Radiographs did not show a significant problem, but the ERG (Fig. 2) showed an abnormally shaped graph with a rating of 65. The filling was removed, revealing a leaking alloy marginal opening, with gross decay across the entire intaglio surface of the filling and a tooth fracture on the pulpal floor that ran halfway from the distal marginal ridge to the center of the tooth.
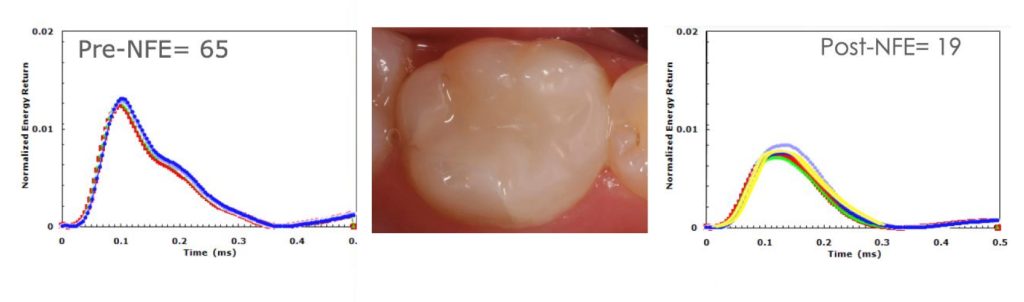
After replacing the leaking restoration with a composite restoration, another QPD measurement was taken and the tooth now registered a rating of 19 (Fig. 3).
(Six years later, the patient moved back to the area and the tooth was tested again. It stabilized at a rating of 21 with no further treatment.)
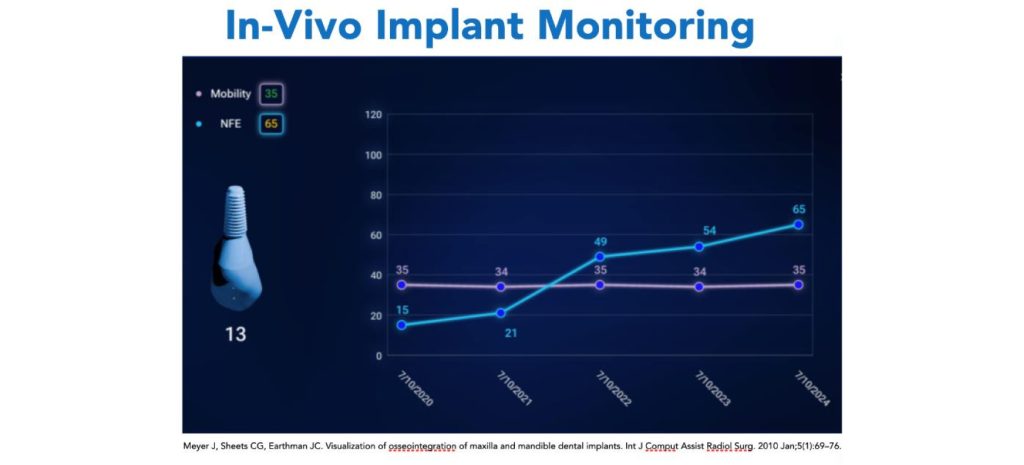
Case 2: An implant defect to evaluate
An annual implant monitoring of a 10-year-old dental implant (Fig. 4) shows a stable osseointegration (purple line). Over the time studied, the implant has had a consistent range of overall mobility between 34 and 35; this reading is well under 51, which represents an acceptable level of osseointegration. The mobility metric is related to the height of the peak in the ERG.
Also charted is another algorithm computed from the ERG that has to do with the shape of the graph (NFE). InnerView refers to NFE as “damage” because it is increased by the internal micromovement of microgap defects in the site; it is thus different from the overall movement of the site. In this example, the implant is stable in its osseointegration, but a defect is exhibiting an increasing oscillation over several years. This could be a loosening cement seal, a loosening screw, or a structural failure in the implant fixture itself. This graph indicates the dentist should evaluate this site more completely.
Technological advantages
One advantage of using a mechanics-based approach to identify structural problems is that it doesn’t depend on image resolution or visual perception. A fractured tooth, a loosening restoration, formerly undetected bone loss, traumatic occlusion, undetected periodontal bone loss, and a beginning pulpal breakdown that affects the periodontal ligament are all examples of difficult-to-see defects that can be detected using QPD, which alerts users to any structural instability and the magnitude of the problem so they can use other clinical aids to better assess why the site is unstable.
No special equipment is required to use InnerView beyond what the implant manufacturer provides: Normal healing caps, impression abutments, premade abutments, custom abutments and even final crowns can be tested. If anything projects high enough to seat the 3-millimeter-diameter tip of the handpiece (Fig. 5), a measurement can be made. It takes 2–3 seconds to test a site, and a little over a minute to measure the entire dentition.

Research and specifics about QPD and InnerView
Research on QPD technologies started more than 18 years ago, and selected investigative offices strategically spread across the country started collecting data under Institutional Review Board-approved studies more than 10 years ago.
Twenty-eight published studies in top international peer-reviewed journals provide a solid research base for understanding the system’s capabilities. (Browse them here.)
Two 510(k) clearances have already been granted, covering all InnerView equipment and software and the first algorithm that measures overall mobility in teeth and implants. InnerView expects to have clearance on NFE, which will measure oscillation micromobility in the internal portions of the tooth or implant, this year.
There are more than 60 issued patents on this technology in the U.S. and other international regions.
Expected technological expansions
Perimetrics has started taking orders for this InnerView system for measuring implant and tooth mobility; delivery of this system will start in late March or April. Additional algorithms in development would help differentiate between hard-tissue and soft-tissue issues; as these are cleared by the FDA, they will be downloaded to the software, automatically updating the equipment.
There are already indications that each tooth and implant’s unique ERG “fingerprint” carries information to help identify unseen maladies within it. In cases with multiple structural problems, the software will eventually be able to provide the probability of different problems within a given tooth or implant.
Being involved in the development of a breakthrough technology is exciting and rewarding. We are grateful for the dedicated team of dentists, engineers, data scientists, and top industry professionals on the journey with us.
Editor’s note: James Earthman, PhD, chief science officer and a co-founder of Perimetrics, also contributed to the writing of this article.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Cherilyn Sheets
Date: February 25, 2025
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


