Comprehensive Alveolar Ridge Augmentation and Implant Placement: A Case Study
Alveolar ridge changes after tooth extraction pose a significant challenge in implant dentistry. The natural resorption process results in a reduction of both horizontal and vertical dimensions of the alveolar ridge, complicating implant placement and necessitating advanced surgical techniques. These changes not only affect hard tissues but also induce significant alterations in soft tissues.
The reduction in alveolar ridge height and width leads to a decrease in vestibular depth, which can compromise the hygiene of the future implant. The reduced depth makes it difficult for patients to clean around the implant effectively, potentially leading to plaque accumulation and increased risk of peri-implant disease. The diminished depth can also affect the fit and stability of dentures or other prosthetic devices, compromising their functionality and comfort.
Additionally, the position and quantity of keratinized mucosa are often adversely affected. The keratinized tissue, which is essential for maintaining a healthy and stable soft tissue barrier around implants, becomes displaced or reduced. This change can result in less stable soft tissue around the implant site, potentially increasing the risk of peri-implantitis and other complications. Inadequate keratinized mucosa can lead to mucosal recession, exposing the implant surfaces to the oral environment and making them more susceptible to bacterial colonization.
Maintaining adequate keratinized mucosa around dental implants is critical for peri-implant health. Keratinized mucosa provides a stable, resistant soft tissue barrier, protecting against mechanical stress and microbial invasion, which is essential for the long-term success of dental implants. Sufficient keratinized tissue also enhances the implant’s esthetic outcome by ensuring a natural appearance of the gingival contour and supporting the soft tissue structure.
The importance of soft-tissue management in implant dentistry cannot be overstated. Achieving and maintaining optimal soft-tissue conditions around implants is vital for preventing peri-implant diseases and ensuring the longevity of the restoration. This involves not only the preservation of existing keratinized mucosa but also the augmentation of deficient areas through grafting procedures when necessary.
This case report describes the comprehensive surgical management of a 55-year-old patient with a significant horizontal ridge defect and minimal keratinized mucosa. The patient required a complex approach to ensure successful implant placement and long-term peri-implant health. The treatment plan involved ridge augmentation, soft tissue grafting, and meticulous surgical techniques to address both hard and soft tissue deficiencies, ensuring a stable and esthetic implant restoration.
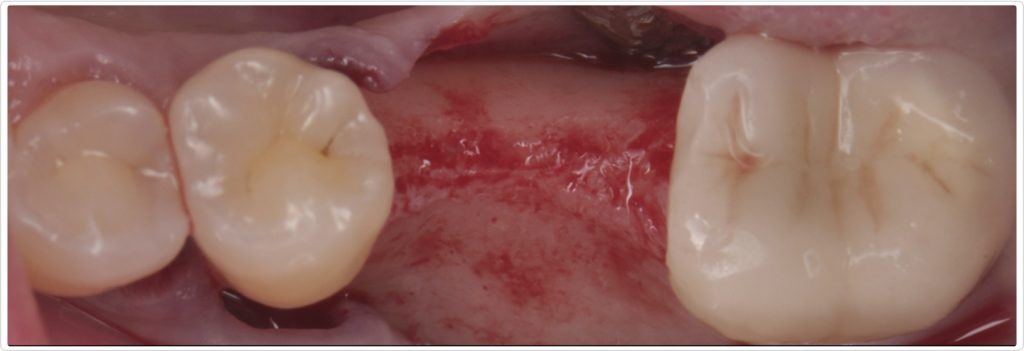
Patient history and initial presentation
The patient, a 55-year-old woman with no significant medical history, presented with an edentulous site in the mandibular first molar region (area #19). The tooth had been extracted more than three years ago because of caries. Initial clinical examination (Figs. 1a and 1b) revealed a horizontal ridge defect and minimal keratinized mucosa at the site, posing challenges for implant placement and long-term stability.

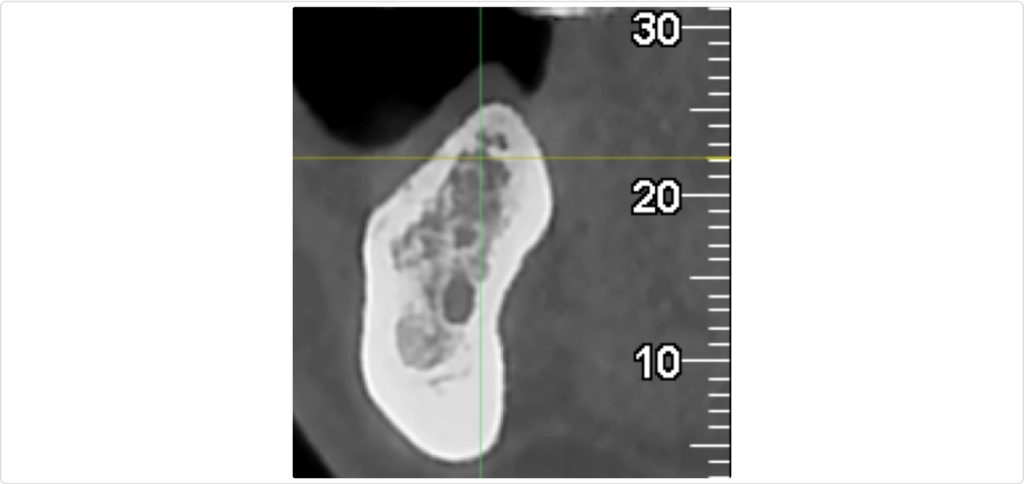
Diagnostic evaluation
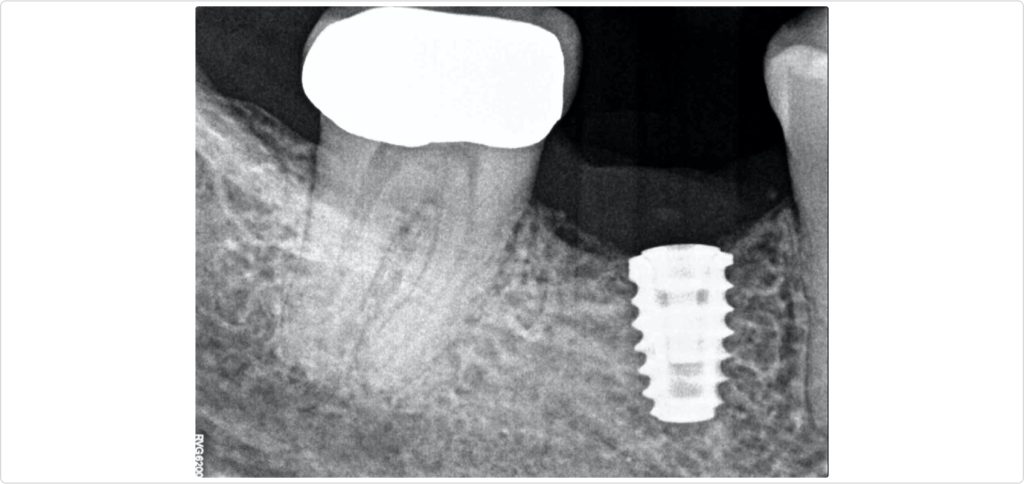
A CBCT scan was performed to evaluate the extent of the ridge defect and the anatomical position of the inferior alveolar nerve. The scan (Fig. 2) confirmed a significant defect and showed that the inferior alveolar nerve was positioned less than 10 mm from the alveolar crest, indicating a high-risk site for implant placement. This necessitated careful planning to avoid nerve damage during the surgical procedure.
Surgical procedure
Flap design and elevation
The surgical intervention began with a crestal incision at the edentulous site, extending to sulcular incisions on teeth #18, #20, and #21 (Fig. 3). A full-thickness flap was elevated beyond the mucogingival line to expose the bone while preserving flap thickness. This approach ensured adequate visibility and access for the bone grafting and implant placement procedures.
A partial-thickness dissection was performed to facilitate flap mobilization and ensure primary wound closure. This technique allowed for sufficient tissue manipulation and coronal repositioning, which is critical for achieving optimal primary wound closure and healing outcomes.
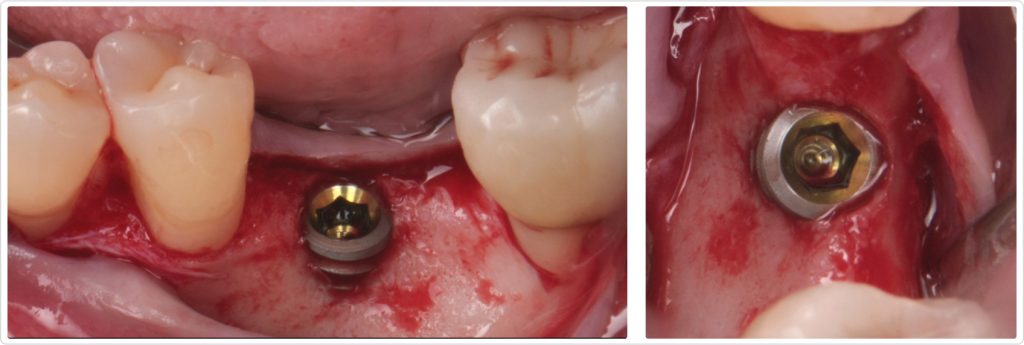
Implant placement and ridge augmentation
The implant (4.6 by 7.5 mm) was placed in an ideal 3D position with an equal distance to the adjacent teeth, 1 mm subcrestal and centered buccolingual (Figs. 4a and 4b). However, because of the significant ridge resorption, approximately 4 mm of the buccal rough surface of the implant was exposed, resulting in a bone dehiscence.
To address this, a cross-linked collagen membrane was used to cover the exposed implant, and a particulate bone graft using freeze-dried bone allograft (FDBA) was applied (Fig. 5). The collagen membrane was secured with resorbable 5-0 sutures anchored to the periosteum, ensuring stability of the graft material and facilitating bone regeneration. This suture stabilized the graft and relieved any extensive flap tension that could have compromised primary wound healing.
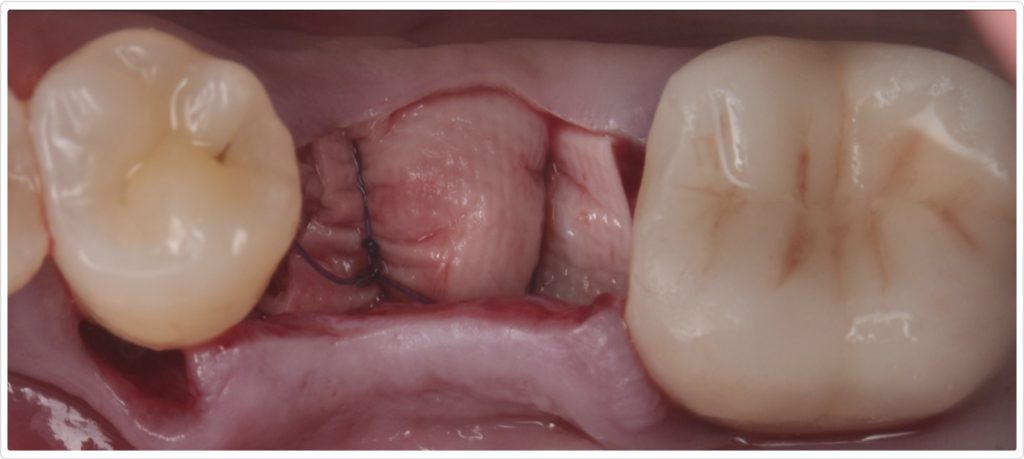
Surgical site closure
The surgical site was meticulously closed using 4-0 PTFE sutures in a horizontal mattress technique, complemented by 6-0 polypropylene simple interrupted sutures in the middle of the ridge to achieve primary closure (Fig. 6). This combination of suturing techniques ensured a stable, secure closure, promoting optimal healing and minimizing the risk of wound dehiscence. Additionally, simple interrupted 4-0 PTFE sutures were used in the interproximal sites.
Postoperative care and evaluation
Postoperative care instructions were provided to the patient, including the use of chlorhexidine rinses, analgesics, antibiotics, and a soft diet to facilitate healing. Regular follow-up appointments were scheduled to monitor the healing process and assess the integration of the bone graft and implant.
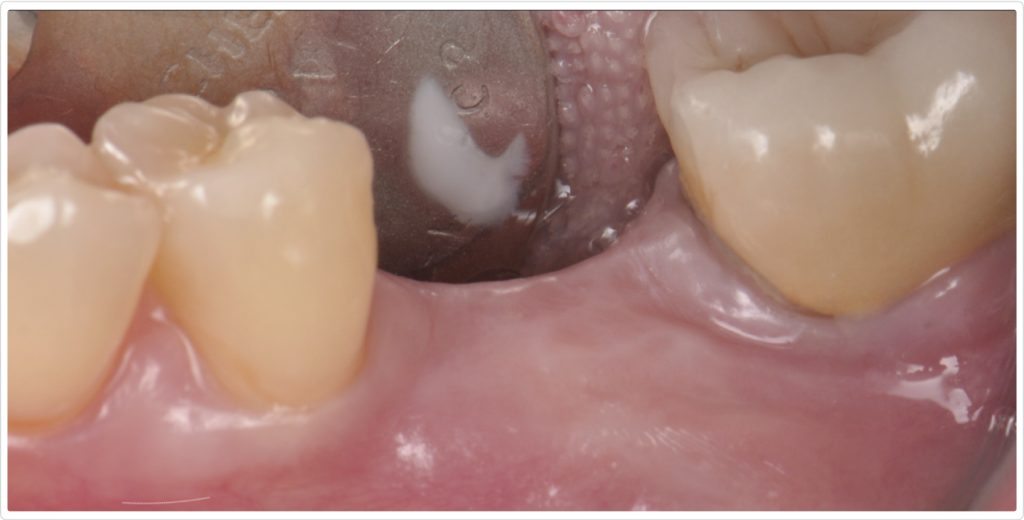
A radiograph taken six months after the procedure (Fig. 7) showed satisfactory healing and bone integration around the implant, indicating successful osseointegration and stability of the grafted site. Clinically, a lateral view of the ridge (Fig. 8) revealed minimal keratinized tissue at the site, highlighting the need for further soft tissue management.
Soft tissue management at second-stage surgery
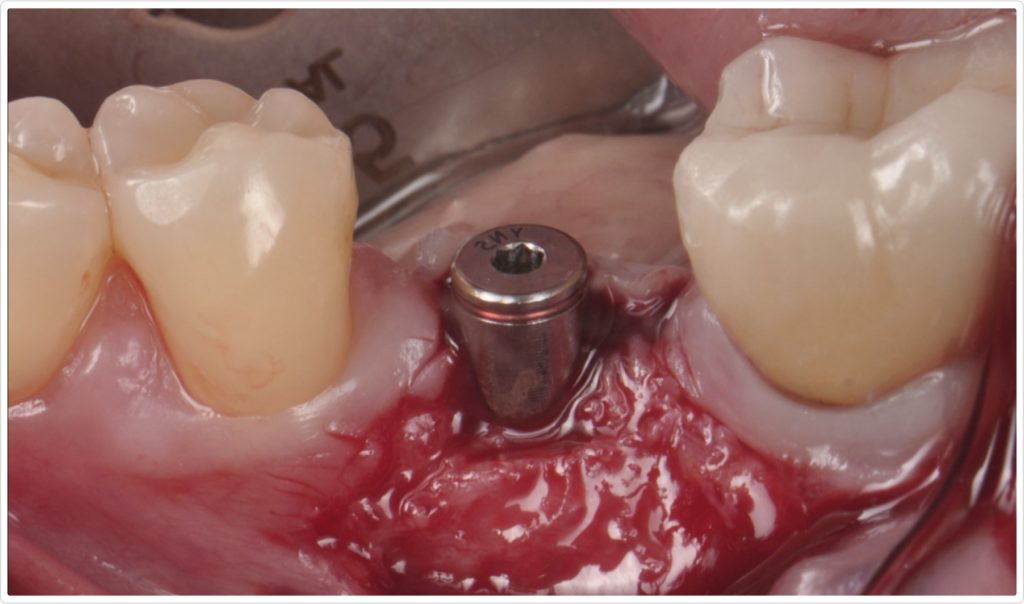
To address the deficiency in keratinized mucosa, a second-stage surgery was planned. A crestal incision was made at the edentulous site, not touching the adjacent teeth. A partial-thickness flap dissection was performed at the implant site, displacing the minimal keratinized tissue present at the lingual site (Fig. 9). Two divergent vertical incisions were made at the buccal area, leaving the connective tissue and periosteum attached to create a vascular surface for a free epithelialized graft. The cover screw was then removed, and a 5 mm healing abutment was placed.
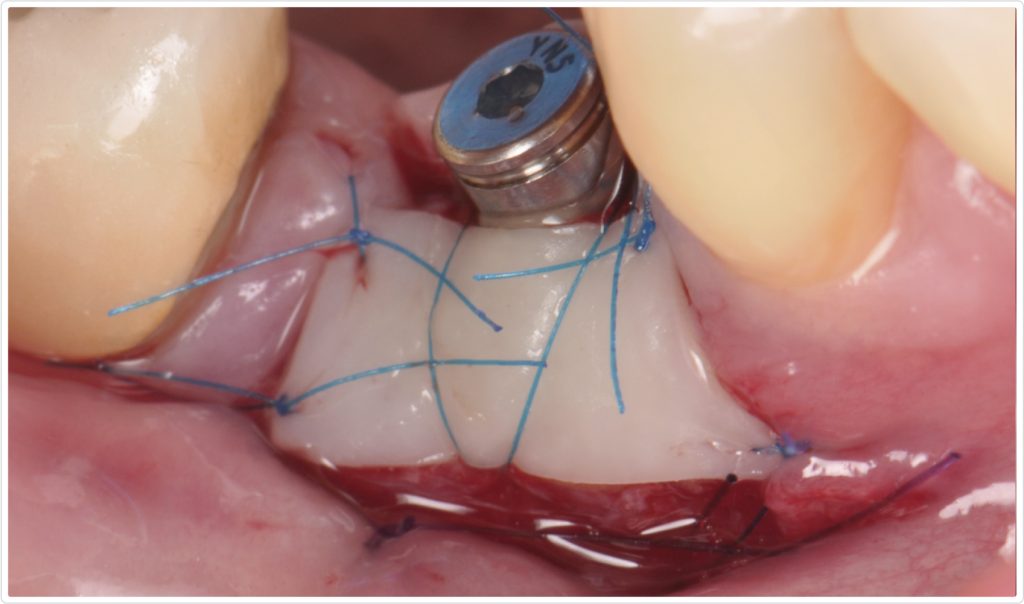
Graft harvesting and placement
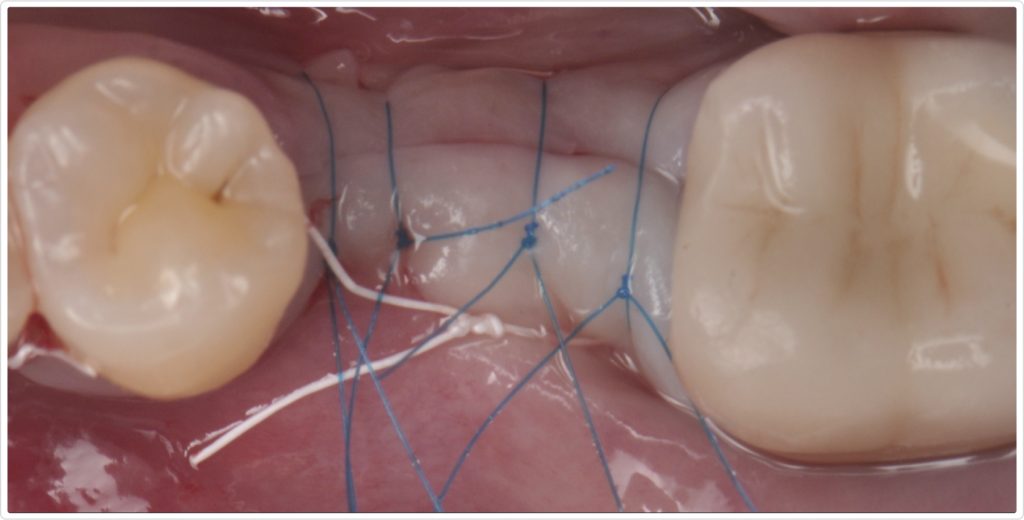
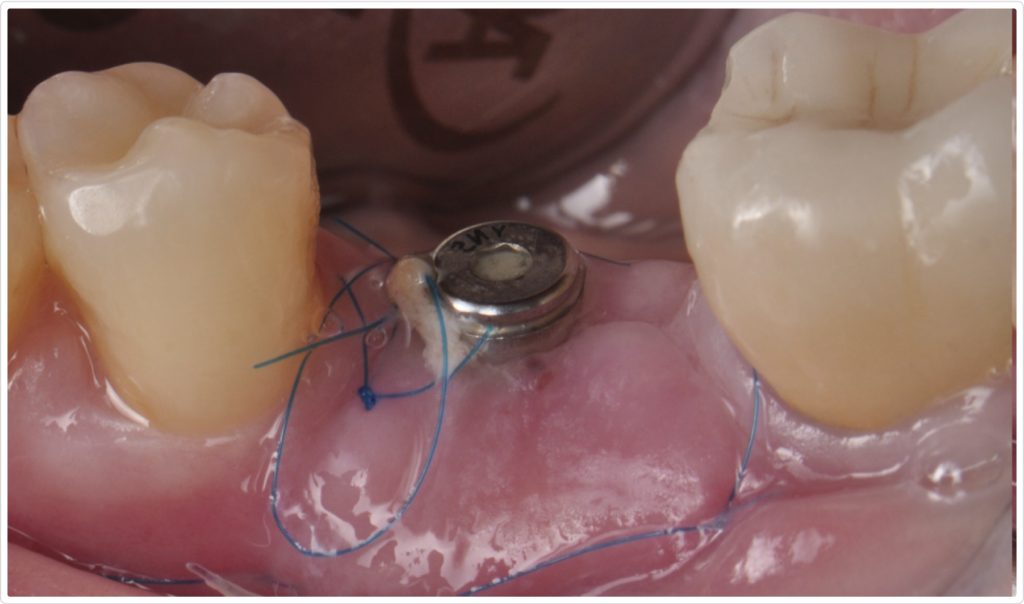
A free epithelialized graft was harvested from the anterior palate and fixed in place with 6-0 polypropylene simple interrupted sutures at the edges and a periosteal suture around the healing abutment. Additional 5-0 simple interrupted sutures were used to secure the flap in an apical position, ensuring optimal adaptation and stability of the graft (Fig. 10). The donor site was treated by means of collagen sponges and crisscross 4-0 PTFE sutures anchored to the teeth, achieving hemostasis.
Healing and final restoration
Two weeks after the procedure, the site exhibited uneventful healing, and sutures were removed (Fig. 11). The patient demonstrated good compliance with postoperative care instructions, contributing to the favorable healing outcome.
Crown delivery
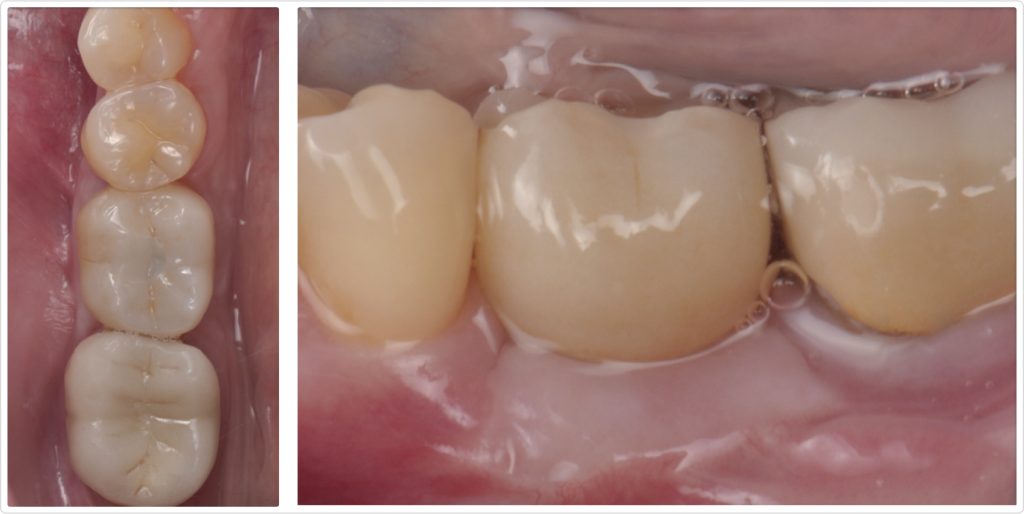
Six months after graft placement, the clinical pictures showed a well-integrated, screw-retained crown with more than 4 mm of keratinized tissue in both occlusal (Fig. 12a) and lateral (Fig. 12b) views. The presence of adequate keratinized mucosa provided a stable and healthy peri-implant environment, which is critical for the long-term success of the implant restoration.
Follow-up visit
A radiograph taken one year after crown delivery (Fig. 13) demonstrated stable marginal bone levels around the implant, confirming the success of the comprehensive surgical approach and the stability of the peri-implant tissues. This radiographic evidence was corroborated by clinical observations, which showed no signs of inflammation or mucosal dehiscence around the implant site. The stability of the bone levels indicated successful osseointegration, a critical factor for the long-term durability and functionality of the implant.

Furthermore, the clinical examination revealed a healthy mucosal contour with an adequate band of keratinized mucosa surrounding the implant. The presence of this keratinized tissue contributed to the overall health of the peri-implant tissues by providing a robust barrier against bacterial invasion and mechanical stress. The patient reported high satisfaction with the esthetic and functional results, noting an improvement in her ability to chew and a significant boost in confidence because of the enhanced appearance of her smile.
Integrated approach, predictable outcomes
This case highlights the importance of a multidisciplinary approach in managing significant alveolar ridge defects and ensuring the presence of keratinized mucosa for long-term peri-implant health. The combination of advanced bone grafting techniques, meticulous soft tissue management, and precise implant placement facilitated the successful rehabilitation of this high-risk site. Using a cross-linked collagen membrane and FDBA particulate bone graft was instrumental in regenerating the lost bone structure, while the soft tissue grafting procedures ensured an adequate amount of keratinized mucosa, contributing to the implant’s long-term stability and health.
The favorable outcome in this patient underscores the efficacy of combining bone regeneration and soft tissue augmentation techniques to overcome anatomical challenges and achieve optimal functional and esthetic results in implant dentistry. Future cases with similar complexities can benefit from this integrated approach, ensuring predictable and sustainable outcomes. By addressing both hard and soft tissue deficiencies, clinicians can enhance the success rates of dental implants and provide patients with restorations that look natural and function effectively over the long term.
Moreover, this case reinforces the necessity of thorough presurgical planning, including advanced imaging techniques such as CBCT scans to assess the anatomical landscape and accurately identify potential risks. The careful planning and execution of surgical procedures and the selection of appropriate grafting materials and techniques are paramount to achieving successful outcomes in complex cases.
In conclusion, managing significant alveolar ridge defects requires a comprehensive and multidisciplinary approach. Integrating bone grafting and soft tissue augmentation techniques is crucial for ensuring dental implants’ long-term success and health. This case exemplifies how a well-coordinated treatment plan, tailored to address the patient’s specific needs, can result in excellent functional and esthetic outcomes, ultimately enhancing their quality of life. As implant dentistry continues to evolve, such integrated approaches will remain pivotal in overcoming the challenges posed by complex anatomical scenarios and delivering predictable, high-quality care to patients.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Gonzalo Blasi
Date: January 7, 2025
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


