Oral Oxidative Stress, Antioxidants and Wound Healing
By Robert Winter on May 5, 2021 | 2 comments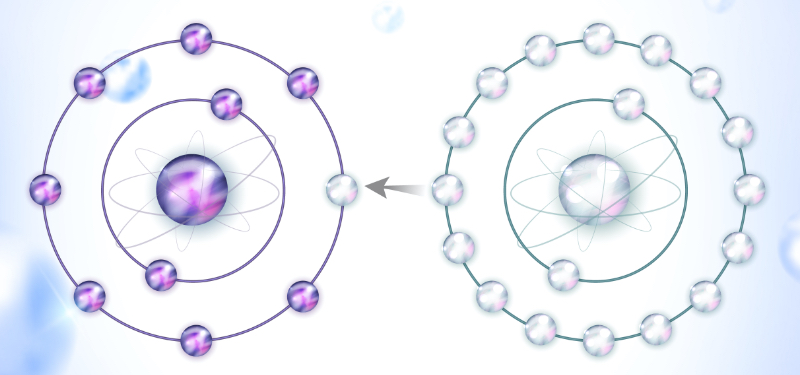
In my last article, “Introduction to Oral Oxidative Stress,” I introduced the process of oxidative stress and how it factors into the development of multiple chronic inflammatory diseases and is suspected to be an underlying cause of oral mucositis in COVID-19 patients.
Here, I will discuss how antioxidants affect wound healing, and how they can be used during patient treatment and home care to improve tissue healing.
Multiple studies have shown a potential decrease in wound healing time associated with the topical application of antioxidants. Specific combinations of antioxidants lower inflammatory markers and facilitate wound healing by promoting fibroblast migration. Their use may be particularly effective in patients who smoke, as nicotine promotes an increase in the production of reactive oxygen species (ROS), which results in a heightened degree of oxidative damage to human fibroblasts.
Infection is another factor that can raise the level of free radicals and ROS. Bacterial infections trigger the release of chemicals including cytokines, chemokines, prostaglandins, and destructive enzymes, which create large quantities of ROS. Viral infections like COVID-19 can cause tissue damage from neutrophil-induced oxidative stress.
Chlorhexidine is commonly used in dentistry post-periodontal surgery to inhibit bacterial infection, but it has been shown to have a detrimental effect on cell migration and long-term cell survival, even in diluted concentrations. Essential oil mouthwashes (menthol and thymol) are a reliable alternative to gingival inflammation and have a comparable anti-plaque and anti-gingivitis effect without damage to cells.
Recently, multiple oral rinses have been recommended for use pre-procedure in the dental office to reduce the transmission of the COVID-19 virus via aerosols. You may want to do additional research to determine the most effective antimicrobial/antiviral products to use in specific situations you may encounter, as new research is being done in this area.
I use a line of products introduced by PerioSciences, L.L.C., that can be used both in the clinical setting and for patient home care to reduce ROS caused by oral stressors. The products work post-periodontal and implant surgery and in restorative procedures that irritate the gingival tissue by increasing cell viability and the migration of fibroblast cells while achieving an antimicrobial effect. They can also be used to help heal ulcers and other types of tissue trauma or injury.
There are specific application regimens for each type of surgery or condition treated. For example, after periosurgery (including implant placement), AO ProVantage Gel is applied three to five times per day for one week, and three times per day during the second-week post-op. A maintenance program after that is recommended. You can contact PerioSciences via its website for information on specific products, regimens, and durations.
Part 3 of this series will address the use of antioxidants in restorative dentistry.
References
- San Miguel SM, Opperman LA, Allen EP, Zielinski J, Svoboda KK. Antioxidant compounds increased wound healing migration via Rac-GTP activation in nicotine-treated human gingival and PDL fibroblasts. Journal of Periodontology. 2010;81(11):1675-1690.
- Allen-Gipson DS, Zimmerman MC, Zhang H, Castellanos G, O'Malley JK, Alvarex-Ramirez H, Wyatt TA, et.al. Smoke extract impairs adenosine wound healing: Implications of smoke-generated reactive oxygen species. American Journal of Respiratory Cell and Molecular Biology. 2013;48(5):665-673.
- Laforge M, Elbim C, Frère C, Hémadi M, Massaad C, Nuss P, Becker C. Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nature Reviews Immunology. 2020;20(9):515-516.
- Van Leeuween MP, Slot DE, Van der Weijden GA. Essential oils compared to chlorhexidine with respect to plaque and parameters of gingival inflammation: A systematic review. Journal of Periodontology. 2011;82(2):174-194.
- Reis IN, do Amaral GC, Mendoza AA, et al. Can preprocedural mouthrinses reduce SARS-CoV-2 load in dental aerosols? Medical Hypotheses. 2021;146:110436.
Comments
May 6th, 2021
May 6th, 2021