If you want to increase the predictability of your restorative treatment plan, incorporate a temporomandibular joint anatomy assessment using CBCT imaging. Here are four big ways a TMJ anatomy assessment can support restorative treatment planning and play an integral role in Great Dentistry.
Condyle size
The first reason is related to condyle size. CBCT can assess condyle size in both a medial-lateral dimension, as well as anterior-posterior dimension. Normal condylar size should be approximately 20 mm (Fig. 1) in a medial-lateral dimension and approximately 8 mm (Fig. 2) in an anterior-posterior dimension.

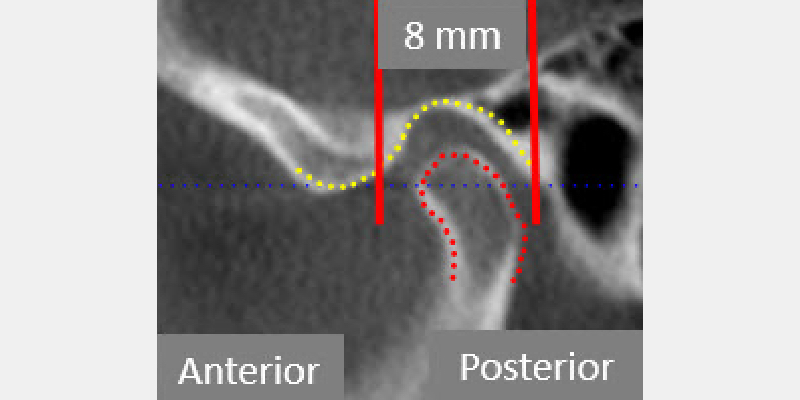
When condyles present smaller than the above dimensions (Fig. 3), the assumption is that it didn't grow to its full genetic potential.

This typically occurs due to an injury to the TMJ, resulting in a disk displacement before growth is complete. Many of these patients will present with a Class II occlusion.1
It's helpful for orthodontic treatment planning to have a clear understanding of TMJ anatomy before beginning treatment for Class II occlusions.
The cortical plate
A second reason for CBCT imaging of TMJ anatomy relates to the cortical plate on the superior surface of the condyle. In the adult patient, the cortical plate should be dome-shaped and be completely corticated (Fig. 4).

Erosions in the cortical plate (Fig. 5) can result not only in pain but also in a loss of TMJ vertical dimension.

The loss of TMJ vertical dimension can present clinically as anterior uncoupled anterior teeth. If the cortical plate in an adult is eroded, it may be advisable to consider appliance therapy before beginning restorative treatment.
The use of a full arch appliance can allow the doctor to track the joint condition through changes in the occlusion on the appliance. The literature states it may take 6-24 months for the cortical plate to remodel and become stable.2
In the growing patient, cortical plate analysis can be used to assess if future growth is possible. In growing patients, the cortical plate is open (Fig. 6), and it is possible to forecast future growth. Once the cortical plate closes, it is unlikely that future growth will occur.

The upper cervical spine
The third reason for TMJ imaging relates to the upper cervical spine. Many patients have misaligned upper cervical spines (Fig. 7) and can present with symptoms similar to patients with TMD problems, so it's important to be able to differentiate between the two problems.
Upper cervical spine misalignment can be easily seen with CBCT imaging and these images can be instrumental in helping patients receive appropriate treatment.

Airway anatomy
Finally, the fourth reason relates to airway anatomy. CBCT imaging allows for an assessment of the nasal septum.
Patients who have a deviated septum may have difficulty breathing through their nose due to the anatomy of the nasal septum. A deviated septum occurs more commonly than generally assumed and understanding septum anatomy can lead to helping patients breathe better.
CBCT can also give insights into pharyngeal airway anatomy. Compressed pharyngeal airway anatomy is often the result of a loss of TMJ dimension. Assessing pharyngeal anatomy through CBCT imaging helps both doctors and patients understand breathing disorders.
CBCT imaging can be obtained in a fully seated condylar position in order to interpolate disk position through assessing the condylar position. There is little diagnostic value in obtaining open view CBCT images since the disk position can be assessed with CBCT.
Lastly, it's helpful to have a radiologist review the CBCT imaging to assess any incidental findings that may present.
Jim McKee, D.D.S., is a member of Spear Resident Faculty.
References
1. Manfredini D. Temporomandibular joint disorders in patients with different facial morphology. a systematic review of the literature. Journal of Oral and Maxillofacial Surgery.2016;74(1):29–46.
2. Bae S, Park M-S, Han J-W, Kim Y-J. Correlation between pain and degenerative bony changes on cone-beam computed tomography images of temporomandibular joints. Maxillofacial Plastic and Reconstructive Surgery.2017;39(1):19.
Comments
August 20th, 2020
August 24th, 2020