Low-Level Laser Therapy In Dentistry - Was 'Star Trek' Technology That Far Out?
By Kevin Huff on October 10, 2018 |Dr. “Bones” McCoy was famous for performing all sorts of life-saving procedures on his patients in the series StarTrek : TOS without ever yielding a blade and using what appeared to be laser technology. At the time that those episodes ran on primetime television in the late 1960s, that technology seemed extremely far-fetched.

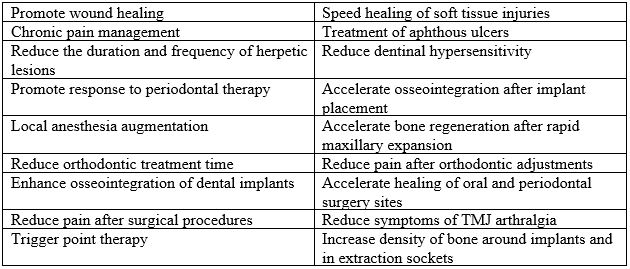
However, within the past decade, low-level laser therapy with lasers that do not touch the tissue have shown promise in sports medicine, veterinary medicine, and now in dentistry for a variety of purposes, including enhanced wound healing and tissue regeneration, promotion of soft tissue injury healing, pain management and a host of other reported uses. (Table 1.)
Even as Gene Roddenberry was dreaming up out-of-this-world medical technologies for his television series that would eventually spawn an entire subculture, low-level laser therapy (LLLT) was being used to stimulate hair growth in mice. While all lasers can be used to deliver LLLT, the most commonly studied laser for this purpose is the diode laser, with wavelengths of 810 to 980nm. While the dosage and strength of laser radiation needed for specific purposes has not been standardized and refined in high-level research studies, some laser manufacturers offer specific recommendations based on their proprietary devices.
However, since the effective dosage of laser radiotherapy depends greatly on the technique used by the operator (circular motion, static delivery, proximity to the site, etc.) and by the phenotype of the target tissues, standardization is difficult. Nevertheless, the general principles of laser therapy that have yielded favorable outcomes include a non-contact mode of laser delivery, typically with a diode laser within the near-infrared spectrum of visible light between 600 and 1100 nanometers. (Figure 2.)
Generally, lower doses given over several sessions for one to three weeks provide better results than aggressive therapies. Some general laser parameters for LLLT in wound healing have been proposed:
- The power output should be between 0.001 and 0.1 Watts.
- Effective wavelengths for LLLT are between 300 to 10,600 nm.
- The pulse rate is continuous (non-gated) or at a frequency of 5000 Hz.
- Laser intensity should be 0.01 to 10 W/cm2 and dose of 0.01 to 100 J/ cm
Calculating all of these powers and dosages may be a daunting task, except for possibly laser physicists. Therefore, it is best to follow the guidelines established by the manufacturer of the laser being used for specific LLLT purposes. Preferably, FDA-approved lasers should be used because they have been cleared as safe for LLLT based on defined guidelines.

How does low-level laser therapy work?
In contrast to a focused laser beam that concentrates photons in order to cut, ablate, or destroy tissue, LLLT is a defocused beam that does not appreciably elevate the tissue temperature and should not destroy tissue. In fact, lasers designed for LLLT are sometimes referred to as “cold lasers.” Lasers work by affecting certain elements within target tissues that absorb specific wavelengths of radiation, which are called chromophores. Soft tissue chromophores are melanin and hemoglobin. Hydroxyapatite is a chromophore of hard tissues. Water is a chromophore for both hard and soft tissues.iii
Interestingly, hypoxic and damaged cells or tissues at risk of death are affected more than healthy tissues. The term “photostimulation” is often used to describe the effects of LLLT, because it tends to stimulate and promote growth and healing of injured tissues. Published effects in various situations have been explained in the literature for several situations.
Injured muscles and trigger points
Along with physical therapy, occlusal orthotic appliances, massotherapy, spray-and-stretch, ultrasonagraphy, medications, injections with local anesthetic and other medications, and electrical stimulation, LLLT (considered a non-invasive modality) has been used to treat muscle fatigue, injury, and trigger point hyperactivity.xii
The proposed mechanism of action is that nitric oxide is released, which temporarily increases blood flow to the tissues and dilates the lymphatic system to improve drainage away from the injured tissue to reduce swelling. Prostaglandin E2 production is decreased and mast cell degranulation occurs, which reduces inflammation.
In painful muscles, inactive enzymes are activated by the light radiation, which increases production of growth factors and regenerative processes intracellularly. LLLT also relaxes vascular smooth muscles to enable increased oxygenation and transport of necessary immunochemistry components to facilitate healing. Macrophages are also activated to increase phagocytosis and clean-up of damaged tissue and fibrin, which in turn leads to increased fibroblast growth facture. Proliferation, increased locomotion and maturation of fibroblasts, which then transform into myofibroblasts, occurs to enable growth of new muscle.
Wound healing
One application of low-level laser therapy with which I have had significant personal experience (and which offers anecdotal support from direct observation) is its significant impact on surgical wound healing. In a clinical setting, complex exodontia with multiple teeth using standard atraumatic techniques (with and without full thickness flaps and sutures) has predictably been performed on multiple occasions over the past five years using immediate post-op LLLT applied to the surgical sites with only one application (3W, continuous, hovering in a circular pattern over the wound with a 1 cm spot size without a tip in a non-contact application using an Odyssey Navigator diode laser - an off-label application).
Using this therapeutic regimen, post-op pain reports from the patients at three and seven days have not exceeded a “two” on a visual analog scale (10 marks on a 10 centimeter line where “10” is the worst pain possible, and “zero” is no pain at all).
These patients have only required two to three days of 600 to 800mg ibuprofen every six hours with 500mg acetaminophen when needed for breakthrough pain, regardless of single extractions or multiple extractions. In fact, these patients have often had to be encouraged to take the ibuprofen because they experience very little pain, but the anti-inflammatory effects of ibuprofen post-operatively are still desired by the clinician.
The literature supports this observation. LLLT releases endorphins to assist with analgesia. It stimulates mitochondria to produce ATP, which increases cell metabolism by 150 percent to encourage growth. Through similar actions (as mentioned in the discussion about muscles above), immune function is improved, inflammation is reduced and edema is minimized. However, the effect of LLLT in extraction sites is dependent on surrounding bone thickness moreso than soft tissue thickness.xi
While dosages and techniques require better standardization based on further research, the conclusion from a meta-analysis of literature reviewing LLLT in wound repair should not be dismissed: “We conclude that laser therapy is an effective tool for promoting wound repair.”v
Nerve injury
LLLT decreases the frequency with which nociceptors stimulate action potentials in the trigeminal nerve, which may explain how analgesia and even pulpal anesthesia occurs in some individuals with LLLT. Also, inflammatory mediator production has been observed to be reduced by LLLT in injured nerves. However, nerve therapy usually involves daily application of LLLT for prolonged periods and at higher doses than other applications (e.g., 10 days at 4.5J per day). When considering the prolonged morbidity associated with surgically-insulted inferior alveolar nerves, LLLT may provide a reasonable approach to therapy.xii
Risk management of LLLT
As with any treatment or therapy that a dentist may provide, informed consent must be obtained through discussion with the patient about reasonably possible risks and benefits of the procedure as well as what might happen without the procedure. Unfortunately, for LLLT, that discussion at the time of this publication must include the fact that further research is needed to better refine dosages of laser radiation for each application. Also, many devices have been cleared for LLLT by the FDA (indicating that they are safe for LLLT) but LLLT can be provided by many different laser devices off-label, and that all of the risks have not been clearly identified. From a general review of literature and courses I’ve taken, as well as from personal experience, the risks seem to be fairly limited to:
- Potential local tissue discoloration
- Mild pain or worsening of symptoms being treated
- Delayed healing of surgical wounds
- Localized tissue burning.
Theoretically, these are likely due to exceeding the appropriate dosage for the purpose intended. However, LLLT is considered to be non-invasive,xii so by definition it carries minimal risk.
Concluding thoughts
Based on the available literature, my clinical experience and that of others, patient interview responses and the meta-analyses of literature cited in this article, low-level laser therapy should be considered to be a reasonable non-invasive option to promote healing and to help reduce post-operative surgical pain. However, further research is needed regarding standardized dosing protocols and specific tissue effects. It is possible that Dr. “Bones” McCoy’s techniques were not so out-of-this-world after all, and maybe Captain James T. Kirk was talking about the dentistry of the not-so-distant future when he said the following in one of the Star Trek: TOS episodes:
“That’s like saying that you wish that you still operated with scalpels and sewed your patients up with catgut like your great, great, great grandfathers used to … Dr. McCoy is right in pointing out the enormous danger potential with any contact with any advancement in science as fantastically advanced as this. But, I must point out that the opportunities for knowledge - for potential - is equally great!”References
I. https://www.google.com/search?q=image+dr+mccoy+treating+patient&tbm=isch&tbs=rimg:CR1zreP-QHVmIjjGGGMeVN9Ub_1tEHW591lx0fi_1XL3OjvocnDIYq4KDqEmCAGJeeXsI0rv2x1_1VfUNBrt5PQi6v1rioSCcYYYx5U31RvEU7u_1DDlccOfKhIJ-0Qdbn3WXHQRzdVKcSvd0BkqEgl-L9cvc6O-hxH6bPRgM7FL2SoSCScMhirgoOoSEeJJvaRxMZVAKhIJYIAYl55ewjQRmyYB1rp_1n_1UqEgmu_1bHX9V9Q0BHJhwmPSVchYSoSCWu3k9CLq_1WuEVLkR-e-6hK6&tbo=u&sa=X&ved=2ahUKEwjG0LmfhZDdAhVlQt8KHWSvAOgQ9C96BAgBEBg&biw=1920&bih=943&dpr=1#imgrc=HXOt4_5AdWY6tM:
II. Mester E, Szende B, Gartner, P. The effect of laser beams on the growth of hair in mice [in German]. Journal of Radiobiology and Radiotherapy (Berlin). 1968; 9(5):621-626.
III. Verma SK, et al. Laser in dentistry: an innovative tool in modern dental practice. National Journal of Maxillofacial Surgery. 2012 Jul-Dec; 3(2):124-132. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3700144/)
IV. Karu TI, Afanas'eva NI. Cytochrome c oxidase as the primary photoacceptor upon laser exposure of cultured cells to visible and near IR-range light. Dokl Akad Nauk. 1995;342(5):693–5. Russian.
V. Woodruff, LD, et al. The efficacy of laser therapy in wound repair: a meta-analysis of the literature. Photomedicine and laser surgery. 2004: 22(3); 241-247.
VI. Posten W, Wrone DA, Dover JS, Arndt KA, Silapunt S, Alam M. Low-level laser therapy for wound healing: mechanism and efficacy. Journal of Dermatological Surgery. 2005;31(3):334–40.
VII. https://www.quora.com/Are-there-colors-that-exist-beyond-the-known-light-spectrum-that-have-not-yet-been-detected
VIII. Bolognani L & Volpi N. Low power laser-ensyme interaction. Laser Applications in Medicine and Surgery. Proceedings of the 3rd World Congress International Society for Low Power Laser Applications in Medicine. Monduzzi Editore. 1992; 213-222.
IX. Karu T. Mechanisms of low-power laser light action on cellular level. Lasers in Medicine and Dentistry. 2000. Vitagraf. 15BN 953-6059-30-4; 108-110.
X. Whelan, et al. Effect of NASA light-emitting diode irradiation on wound healing. Clin Laser Med Surg. 2001, Dec; 19(6):305-314.
XI. Ng, Doreen Y, et al. A pilot study of laser energy transmission through bone and gingiva. JADA. August, 2018; 149(8): 704-711
XII. Munguia, Fernando M, et al. Efficacy of low-level laser therapy in the treatment of temporomandibular myofascial pain: a systematic review and meta-analysis. Journal of Oral & Facial Pain and Headache. 2018.; 32(3) 287-297.
(Click this link for more dentistry articles by Dr. Kevin Huff.)
Kevin D. Huff, D.D.S., Spear Moderator and Contributing Author - www.doctorhuff.net
With so many dental practices, what sets yours apart?
You've grown up, but has your practice? Technology can play a big part in your dental practice's growth. You and every member of your team must understand the value of that technology – and know how to communicate that value to patients. Watch the entire Technology in the Restorative Practice curriculum with a free Spear Online demo.
SCHEDULE FREE DEMO