Lip, Tooth, Ridge Classification Part 3: Space and Tissue Deficiencies
By Ricardo Mitrani on August 26, 2017 |The previous article in this series discussed a couple of different scenarios involving patients with varying levels of space and tissue deficiencies. We will now take a look at the last two scenarios in our arsenal to round out our overview of LTR classification and how it can be used to inform a comprehensive evaluation of our patients’ condition.

Class III horizontal defect
This clinical situation represents a tissue deficiency with a mostly horizontal component, causing inadequate lip support.

For this reason, this situation necessitates a removable prosthesis with a labial extension/flange.


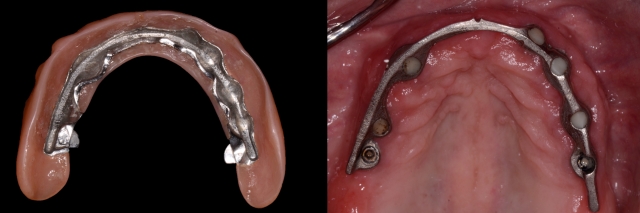
This type of prosthesis (overdenture) can be retained by telescope (Fig. 5) or Locator® attachments (Fig. 6).


Note that the minimal vertical space required for these prosthetic designs is larger compared to that of a Class I, ranging from 11 to 12 mm depending on the system selected. A bar type overdenture may not be recommended for this clinical scenario due to vertical space constraints.
Class III can be converted to a Class IV by means of an ostectomy - however, in cases where such bone reduction is simply not a viable option, anatomical limitations such as a floor of the nose or sinus should be taken into account.
Also, because of the limited vertical space, it’s neither wise nor possible to use a fixed detachable prosthesis. The use of such a prosthetic design would result in a structurally weak prosthesis that will eventually lead to biomechanical complications.
Class IV combined defect
This clinical situation depicts a substantial residual defect (with a vertical and horizontal component) with inadequate lip support. This means we would need a removable prosthesis with a labial extension (flange) with the option of using either the aforementioned prosthetic design for Class III or the utilization of a bar type overdenture.
If a fixed detachable prosthesis were used for this clinical condition, the buccal shelf would compromise access to adequate oral hygiene. Additionally, long-term maintenance of the implants would be at risk and could lead to biological complications.
Space constraints have long been a problem in restorative dentistry, but it’s a problem that can be addressed by increasing vertical dimension and/or by means of surgical bone reduction. Of course, it’s important to note that both alternatives have limitations, be they esthetic, biological and/or structural.
Creating optimal space by removing bone is a common procedure, but it should be cautiously examined; the high biologic cost of removing sound hard tissue “in the name of space optimization” for a certain prosthetic design must be well understood and explained to the patient.
The preoperative evaluation of a patient's existing condition should be a comprehensive exercise. In fact, this is essential in order for the interdisciplinary team to objectively choose the best and most conservative option based on the patient's specific anatomical characteristics. While modifying them to fit a certain restorative design may provide financial benefits, it may add up down the line through the high biologic downside it may incur along the way.
(Click this link for more dentistry articles by Dr. Ricardo Mitrani.)
Ricardo Mitrani, D.D.S., M.S.D., Spear Faculty and Contributing Author
References
- Pound E. Utilizing speech to simplify a personalized denture service. J Prosthet Dent. 1970 Dec;24(6):586-600.
- Frush JP and Fisher RD. The dynesthetic interpretation of the dentogenic concept. J Prosthet Dent. 1958 8(4): 558-581.
- Carlsson GE, Bergman B, Hedegard B. Changes in contour of the maxillary alveolar process under immediate dentures. A longitudinal clinical and x-ray cephalometric study covering 5 years.Acta Odontol Scand. 1967 Jun;25(1):45-75
Save $200 on Our Edentulous Seminar
Eager to master the essentials of treatment planning the terminal dentition and fully edentulous patient? The time is now - secure your limited-time voucher now to save $200 on registration.
REGISTER NOW