Two Steps to Better Bonding in Dental Restorations
By Gary DeWood on February 16, 2016 | Bonding is a vital part of daily practice for every dentist on the planet. It’s a predictable and reliable tool that has dramatically changed what we are able to do for our patients and for ourselves.
Bonding is a vital part of daily practice for every dentist on the planet. It’s a predictable and reliable tool that has dramatically changed what we are able to do for our patients and for ourselves.
Technology has made it possible for us to stick things onto teeth with the expectation that they will stay stuck, a radical departure from the days of my training when resistance and retention form were the only way to keep things from coming off. As the march of progress continues, we have created not just better bonding to teeth, today we are able to stick things to ceramics and metals, too, and we do, hundreds of thousands of times every day. Dentistry is a better profession because of our ability to BOND!
Every advancement in technology brings with it things that we may not have visualized in our excitement to do things better. The predictable reliability of today’s bonding materials is a godsend when we want things to attach well and stay attached for very long periods of time to everything that they touch. This is a considerably less exciting quality when that resin is in places where we have to get it off. Anyone who has struggled to remove the excess bonding material that is attached to a tooth and/or a restoration after placing a beautiful set of veneers is very aware that this bonding stuff really works. It’s perfect for the restoration/tooth interface, a real pain in the neck (and everywhere else) when it sticks to places other than where we want it.


Fortunately, there are two simple steps every clinician can take to minimize this highly frustrating and incredibly tedious task. Step one: careful and judicious use of etchants. Step two: careful and judicious use of silane and silanators.
Seating cases, particularly those that are bonded, is the most highly stressful thing that I do – without exception. I work with WinterLab, a choice that has effectively removed 99 percent of the stress I used to feel about checking for fit and contact before seating. Two days prior to penning this article, I seated 10 units and did not need to adjust any contacts prior to bonding and only had to adjust a few occlusal contacts after.


That is the norm, it’s what I now expect when every case is returned. If you work with a lab and technician who provides you with that same level of expectation, you know what I mean when I say that the feeling in my stomach as I try things in is just not there anymore. Since the addition of these steps into my bonding protocol, the stomach feeling is also much less when the actual bonding begins, although it never goes completely away.
Step 1: Etchants


Step one in our quest to bonding zen is about ACID. Etchants are designed to do exactly what their name says they do. Placed on enamel, they remove a portion of the surface upon which they lie, creating additonal surface area and creating shapes that provide micro-mechanical retention for materials that can fill in those shapes. Placed on dentin, etchants remove the smear layer and create “receptive” collagen fibers, allowing for the creation of a hybrid layer.
(Click this link to learn more about acid etching of ceramic before bonding.)
While phosphoric acid is the best enamel etcher, and the one used on dentin since we started bonding, recent developments have created other acids that work better than phosphoric acid in preparing the dentin surfaces for primers and bonding resins. These newer etchants are placed on the dentin and not removed. We know them as “self etchers.” Their effect on the dentin is the same – disruption of the smear layer and creation of a collagen substrate that can become part of a hybrid layer connecting the dentin with a resin material, generally a “cement” or a composite restoration. These self-etching acids do not perform as well on enamel, but on dentin they are rapidly becoming the state of the art. It is not within the scope of this article to discuss the various ways they accomplish the bonding goals, for our purposes let us accept that they work. In fact, let us accept that they work very well on dentin and pretty well on enamel.
(Click this link for an article on the risks of total-etch systems.)
That my friends is the first genesis of our potential problem. When etch or self-etchers get on parts of the tooth that you do not want to bond to, they do not know you don’t want them to work there, so they do.
Step 2: Silane
 Step two in our quest is about SILANE. Silane and silanators are designed to chemically adhere to ceramic materials. Originally formulated to attach tiles onto the space shuttle, shielding the craft from the heat created by the atmosphere upon re-entry, the applications in other fields quickly became self-evident. In dentistry it moved us from a micro-mechanical to a chemical bond capability that when combined with the micro-mechanical proved more than adequate to connect resins reliably to ceramics for uses in restorative dentistry. Today it is not at all uncommon to design a restoration that has no other way to stay on the tooth than the resin that is bonded to both enamel/dentin and ceramic.
Step two in our quest is about SILANE. Silane and silanators are designed to chemically adhere to ceramic materials. Originally formulated to attach tiles onto the space shuttle, shielding the craft from the heat created by the atmosphere upon re-entry, the applications in other fields quickly became self-evident. In dentistry it moved us from a micro-mechanical to a chemical bond capability that when combined with the micro-mechanical proved more than adequate to connect resins reliably to ceramics for uses in restorative dentistry. Today it is not at all uncommon to design a restoration that has no other way to stay on the tooth than the resin that is bonded to both enamel/dentin and ceramic.
My early protocol for applying it was always to flood the interior surface of the restoration and blow air to dry it. Silane runs over surfaces very quickly when applied, and inevitably the material would spread well past the intaglio surfaces and onto the glazed surfaces that are the exterior of the restoration. It turns out that silane likes those surfaces, too – something that can be a bad idea for restorative dentistry and the second genesis of our potential problem.
After preparing the tooth and the restoration for the goo, positioning the restoration perfectly, and then light curing the goo to create a rock-hard, fully bonded connection between tooth and ceramic, the fun is just getting started. After the stress of getting these things bonded into place correctly, I then spend the next three or four days picking off pieces of bonding cement from around the margins, from the root surface, from the galzed restoration, from the light fixtures … well it seems like three or four days. Imagine the joy when you are able to simply “flick” the pieces off with a scaler, an explorer, and with floss. Ahhhh …. now that is bonding ZEN.

Problem Solving
If you want to take your bonding clean-up experiences to Nirvana, begin by not etching things where you do not want the goo to stick. This seems pretty self-evident, but it is not the way most dentists use etchant. They slather it on all over the place and then rinse it off. Only place phosphoric acid on the enamel that you want goo to stick to. Apply it carefully rather than just squirting it or brushing it on willy-nilly. You will thank yourself later.
Same for the self-etchers. Don’t get them where you don’t want things to stick since they etch whatever they touch. If you blow them thin and they spread onto the tooth past the margins, don’t be surprised when you are pickin’ with that 12 blade for awhile wherever that stuff blew.

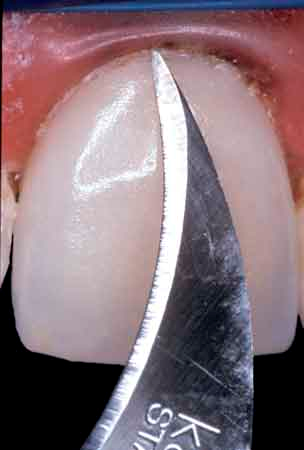
Managing the tooth part of the bonding controls half of the problem. The other half is the restoration and the application of silane. Keep it to the places you want cement to stick to. I use magnification and those little stick things that let me grab the restoration and hold it so I can see it. I do not blow air on it; I let it air dry. Due to something I heard from someone, somewhere, I apply two coats. I’m not sure this does anything other than make me feel good, but it does make me feel good, so I do it.

So, do these two things:
- Do not etch where you don’t want it to stick
- Do not silane where you don’t want it to stick
Welcome to Nirvana.
(Click this link for more clinical articles by Dr. Gary DeWood.)
Gary DeWood, DDS, MS, Spear Faculty and Contributing Author
Resources
Passia, N, Lehmann, F, Freitag-Wolf, S, Kern, M. Tensile bond strength of different universal adhesive systems to lithium disilicate ceramic. The Journal of the American Dental Association. 2015;146(10):729–734.
Giannini, M, Makishi, P, Ayres, APA, et al. Self-Etch Adhesive Systems: A Literature Review. Brazilian Dental Journal Braz Dent J. 2015;26(1):3–10.
SPEAR ONLINE
As a Spear member, you can assign a Spear Online practice delegate to assign courses, track team progress and edit team member accounts on your behalf. Check out the “Getting Started with Team Training” guide to learn more about how a team training partner can help you achieve your goals with Spear Online.
LEARN MORE