7 Steps to Using Retraction Cord When Making Impressions
By Mary Anne Salcetti on November 16, 2015 |One of the most challenging aspects of crown and bridge treatment is the management of the gingival tissue prior to impression making.
The management includes placing the gingival tissues away from the prepared tooth margins so that they can be impressed, combined with providing for hemostasis when the gingival tissues might bleed. Whether or not the impression is made conventionally with impression material or with a digital impression technique, all the tooth margins need to be captured to assure an excellent marginal fit of a lab fabricated restoration.
There are many techniques to achieve retraction, including retraction cords, chemical reagents, electrosurgery, laser tissue sculpting and hemostatic materials that displace tissue atraumatically. In most cases, gingival retraction cord is the most effective and most commonly used method. Controlling the soft tissue, managing any bleeding and exposing the margins is what is most critical. That is why the clinician needs to understand all the choices available. One might choose different alternatives depending on the tooth being impressed.
Mechanical displacement of the gingival tissues aside from the tooth prep margins allow us visualization and access, and we do this best with retraction cords. A survey of prosthodontists in 1999 showed that 98 percent of those who responded used retraction cord and half of them used the double cord technique. Back then, plain cord was the most commonly used cord followed by aluminum chloride-impregnated cord.
Types of Cords: Braided versus Knitted

Knitted cords unravel and fray less when cut during placement, so it’s theoretically easier to place. Since they expand when wet, knitted cords will open the sulcus greater than the original diameter of the cord.
With either braided or knitted there is a variety of diameters and sizes to allow for ease of placement in tighter and healthier gingival sulcuses. Ultimately, it is a personal preference.
One study published in the showed that knitted cords were preferred over braided and there was no advantage to cords impregnated with epinephrine.1 It usually becomes a person’s preference as to what exactly is desired. Either way, when handling retraction cord it is important to remember to use latex free gloves because contamination of the cord with latex can have a deleterious effect on the setting of the VPS impression materials. This is important when a light body material is placed first into the sulcus. If it does not cure completely, it can result in inaccuracies or tearing of the fine gingival margin within the impression.
Cord Packing Instruments

Many clinicians find that placing the cord with a nonserrated instrument easier as the cord won’t pull back out of the sulcus. Design of the instrument is limited to the manufacturer, but many dentists utilize two different instruments depending on the tooth location. Thin, flat instruments for anterior tissue (which tends to be thinner and tighter) works quite well, and rounder serrated or non-serrated work better for posterior teeth.
Astringents/Hemostatic Agents
The astringents cause a contraction-retraction of the tissues, and the hemostatic agents constrict blood flow through coagulation. These agents will initially cause a transient ischemia shrinking the gingival tissue. These compounds include aluminum potassium sulfate, aluminum sulfate, 20-25 percent aluminum chloride, 15.5-20 percent ferric sulfate, and racemic epinephrine (4-8 percent).
We do know that chemically impregnated cords offer better sulcus displacement as you have both a mechanical and chemical effect. When used for durations of less than 10 minutes, they cause minimal tissue damage. These chemicals can interfere with the surface detail of the impression material and with the dentin surface, so thoroughly cleaning the dentin before using a resin bonded cement is recommended. (Click here for tips on choosing impression materials.)
Racemic epinephrine impregnated cord can cause elevated heart rate, blood pressure (especially if placed into bleeding tissues), and literature shows there is no clinical benefit in gingival retraction with this. But if you still choose to use them, the 4 percent is safer for cardiac patients than 8 percent.2
One study examined the effect of presoaked cords on the microcirculation of the tissue at the gingival margin and found that blood perfusion fell markedly upon inserting the cord (with all the compounds). However, after five minutes the decrease became less apparent with cords impregnated with the ALCL3 and Fe2(sSO4)3. The epinephrine-soaked cord continued to affect blood flow for the next 20 minutes. 3
The consensus seems to be that using presoaked cords is more convenient than cutting, soaking and blotting before placement. Remember that ease in placement process is desirable.
Finally it must be noted that these agents are acidic ranging from 0.7 to 2.0. They can remove the dentin smear layer and can cause post-op sensitivity, so be sure to use a cleansing and desensitizing agent.
Cordless Retraction
I have been a huge fan of these products as they deflect tissue and control hemorrhage and moisture. It’s also so much easier to syringe it in (less time and force) than pack cord in. If you have deep subgingival margins, these products don’t work as effectively.
I have used these products and find that they work pretty much the same. Expasyl, Traxodent and GingiTrac are probably the most popular ones. They are made from a viscous paste of diatomaceous clay with aluminum chloride and require two minutes in the sulcus. They give excellent retraction that is non-traumatic and non-invasive. When used with a compression cap, they enhance the effects of the material. They can be used alone or with retraction cord.
How to Do It
First of all, there is no one size fits all.
- Evaluate the health of the gingiva and the depth of the sulcus. Select a diameter that looks like it will fit. If there is minimal sulcus depth, it will only accommodate a single cord technique and probably only a thin cord. A deeper sulcus with healthy tissue accommodates a double cord technique (thin in first followed by a wider diameter). The initial thinner cord controls any bleeding from the base of the sulcus. The cord works mechanically, but the stringent has the function of blocking sulcular secretion and hemorrhaging.
- Twist the first cord very tightly and loop it around the preparation. Overlap slightly and gently tuck it down beneath the shoulder of the prep. The cord will unwind a little bit and force the tissue laterally away from the tooth.
- Next, twist the second cord tightly and repeat the process. Again the cord will unwind slightly and force the tissue laterally.
- Leave the cords in place three to five minutes.
- Right before making the impression, the cord should be wetted with water so it won’t grab and tear the tissues when it is removed, creating more bleeding.
- Once the cord is removed, the retraction is maintained for 30 seconds. Be prepared to begin immediate syringing of your impression material. If bleeding is persistent when the first cord is removed, go ahead and make the impression anyway knowing it won’t be acceptable (don’t even look at it), but it will maintain retraction and give hemostasis. Once you remove it, immediately make a second impression as the sulcus will be open and not be bleeding. It does take more time and expense to do the double cord technique but many feel the accuracy of the impression makes it worthwhile.
- Some clinicians prefer to put the retraction cord in before finishing the preparation. Dragoo and Williams reported that this produced minimal gingival lesions and the best tissue results for operative procedures.
When we compare cordless and conventional displacement systems, the results of one study showed that non-impregnated displacement cord was the least effective in terms of bleeding and impression quality. So if you are placing cord, use an astringent with it. Using a retraction cap with paste showed better results for ease of application, time spent and bleeding management than aluminum chloride cord. Using both the aluminum chloride cord and paste-cap it showed the best results for tissue management and impression accuracy, but was time consuming and difficult. So except for the non-impregnated cord group, all groups are comparable and clinically useful.
Ultimately, the most appropriate technique for the clinical situation is based on your comfort with your clinical skills, your knowledge, and your commitment to understanding that your choices will influence the accuracy of the impression and the response of the tissue.
When thinking about gingival retraction techniques, think about having a few options in your armamentarium to choose from. The tissue, the time and the ease of placement will probably determine how you will decide what you will do. All will work well if done well.
Lastly, who decides what cord to buy in your office? Is your purchasing assistant buying a “special” that you may never use or has no idea what the differences in the astringent agents are? How many cords do you really need and routinely use? Make sure your asking yourself these questions. It is worthwhile for all clinicians to review their protocol and understand all the choices available.
References
- Clinical trial of gingival retraction cords. J Prosthetic Dent. 1999 Mar; 8(3):258-61
- Human blood pressure and pulse rate response to racemic epinephrine retraction cord. J Prostate Dent. 1978 Mar; 39(3):287-92
- Effects of pre-soaked retraction cords on the microcirculation of the human gingival margin. Oper Dent. 2002 Jul-Aug; 27(4):343-8
(If you enjoyed this article, click here to read more by Dr. Mary Anne Salcetti.)
Mary Anne Salcetti, DDS, PC, Spear Visiting Faculty. www.maryannesalcettidds.com
FREE COURSE:
Implant Impression Copings and Impression Techniques
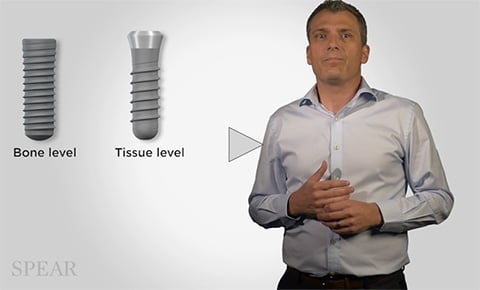
Now that you've learned more about making impressions using retraction cords, check out this free course on implant impression components and applications. In "Implant Impression Copings and Impression Techniques," we cover selecting impression components for Straumann Bone and Tissue Level implants.
WATCH NOW