The Ideal ‘Reduction Sauce’ for Restorative Success With Posterior Ceramic Onlays
All-ceramic posterior onlays are a fantastic restorative solution. For patients in need of cuspal coverage, these restorations provide several benefits, including:
- Conservative tooth reduction
- Supra-gingival restoration margins
- Ease of patient maintenance
- Improved esthetics
- Adequate strength for longevity
Success with posterior onlays is dependent upon adequate tooth reduction to provide long-term strength and durability. Teaching in Spear’s Restorative Design workshop, Dr. Bob Winter and I commonly hear frustrations from attendees who desire to integrate posterior ceramic onlays into their practices on a routine basis but are concerned about ceramic fracture.
Many participants have attempted ceramic onlays for their patients, but, unfortunately, have experienced onlay fracture within months of insertion. These experiences prevent the dentist from pursuing further posterior ceramic onlay restorations.
Many of us have faced this issue while exploring new technologies, materials, or procedures. Understanding how and why these failures occur enables us to move forward with newer concepts with greater confidence and success.
Why Thickness Matters for Ceramic Onlay Success
There are two main components to predictability with ceramic onlay success. The primary component is an adequate thickness of ceramic material to withstand the forces of occlusion and function. This is the primary topic of this article.
Second is ceramic adhesion. Long-term success with ceramic restorations is also dependent upon proper bonding and adhesive protocols. This topic is covered extensively in both the Restorative Design and Anterior Restorative Dentistry workshops at the Spear Campus. I will limit this article to the key concept of tooth preparation and ceramic thickness.
While teaching a recent Restorative Design workshop, I had another conversation about ceramic onlay predictability with Dr. Matt Nadler of New York. He wanted to integrate ceramic onlays into his restorative practice but was concerned about restoration fracture and longevity.
Additionally, Dr. Nadler and I discussed food and food preparation. It occurred to me that proper preparation was the key to excellent results for both food and ceramic onlays. The “concept of the “ideal reduction sauce” ideal reduction sauce” concept for ceramic onlays stems from this conversation with Dr. Nadler (Thanks, Matt!).
In the culinary world, reduction sauce is “the process of intensifying and ‘thickening’ a liquid mixture, such as soup, wine, or juice, to improve the flavor and enhance the product.” This definition is totally appropriate for application to ceramic onlays.
“Thickening” is the key ingredient in improving or enhancing the product. In other words, adequate ceramic thickness provides predictability and success for the final restoration.
The “Restorative Design” workshop provides three full days of understanding and application of preparation design and process for all ceramic restorations. Veneers, crowns, and partial coverage restorations are covered in extensive detail. This article will emphasize the importance of adequate occlusal reduction for posterior partial coverage ceramics. Again, it’s all about the “thickness!”
In most circumstances, partial coverage ceramics are utilized to replace old amalgams, leaking composite restorations, or worn and eroded teeth. When significant tooth structure remains, a more conservative partial coverage restoration is the ideal choice for repair and rejuvenation over full-coverage crowns.
From Diagnostic Wax-Up to Long-Term Results
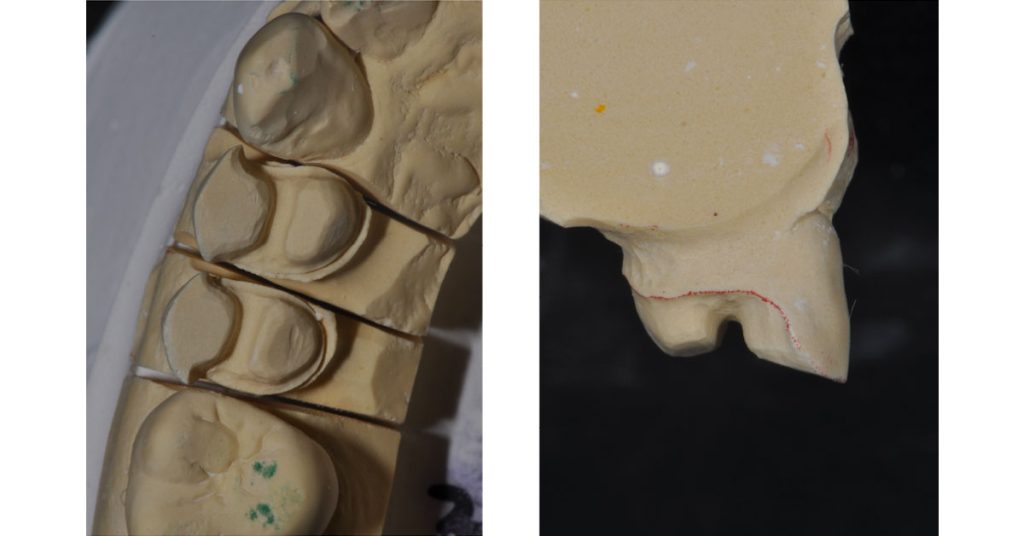
The first step in the preparation process is to design the proposed restoration contours of the finished product. We term this “outcome-based design.” The ideal tooth form, cusp, and fossa heights and contours are established in the diagnostic wax-up. This preview is studied and utilized as a model to prepare and adequately reduce the tooth structure to provide the proper thickness of the ceramic material.

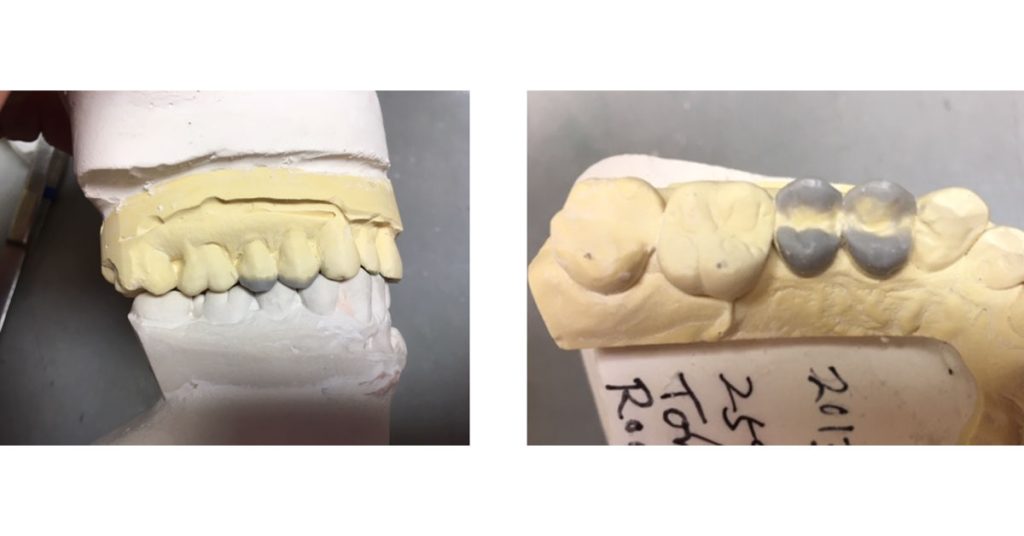
The photos above show the pre-treatment tooth and the required cuspal coverage due to enamel erosion. The diagnostic wax-up provides a preview of the desired outcome. Note the cuspal height changes that are to be incorporated into the final restoration. This is a key observation! Ceramic restoration failures occur due to inadequate reduction related to final-outcome contours.
Adequate reduction is the key to long-term ceramic, partial-coverage restorations. Whether the ceramic is Zirconia or Lithium Disilicate (e.max), the minimal thickness required for material strength is 1.0 mm (bonded to enamel). Many variations in material, thickness, tooth position, and function contribute to altering the overall material thickness, but 1.0 mm is considered the bare minimum.
Ideally, 1.5 mm provides greater predictability and longevity, especially if the restoration is bonded to dentin. Thicker is not always better, but conservative dentistry is a key factor in applying and implementing partial coverage ceramic restorations.
Over-reduction has limitations in some circumstances, as thicker ceramic may cause a loss in perceived value. Again, the many nuances of ceramic preparation and design are covered in detail in the Restorative Design workshop.
I refer you to the following diagrams:
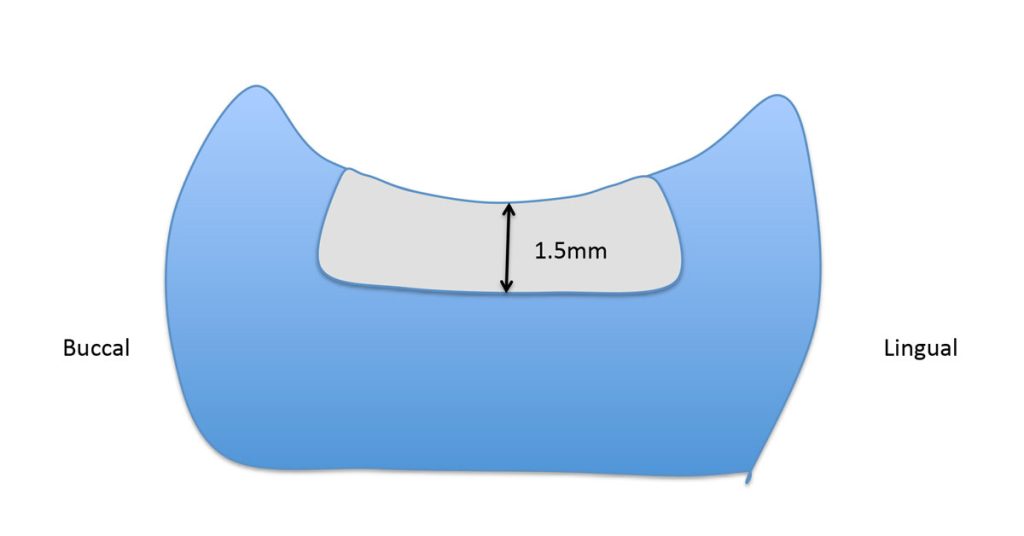
Diagram 1 represents a typical tooth needing occlusal restoration due to wear, erosion, or an old, under-contoured restoration. The occlusal aspect of the tooth is “bowl-shaped.” Sometimes, old amalgam restorations are called “thumbprint amalgams” due to their lack of occlusal anatomy.
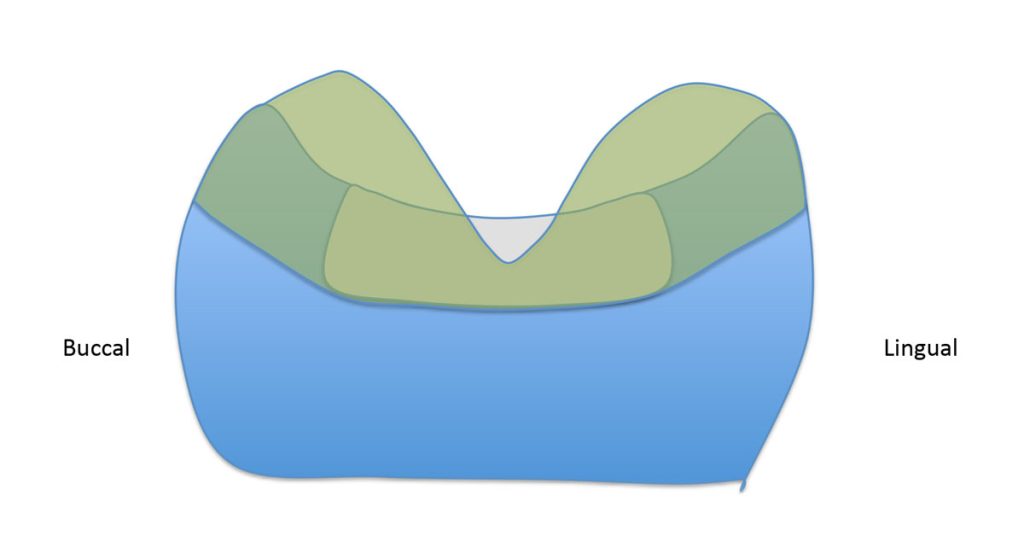
Diagram 2 is of the diagnostic wax-up, or the “proposed outcome” contour of the final restoration. The restoration proposal has integrated significant changes in occlusal anatomy and cup height. These changes must be considered in the tooth preparation to provide adequate thickness for the partial coverage ceramic onlay.
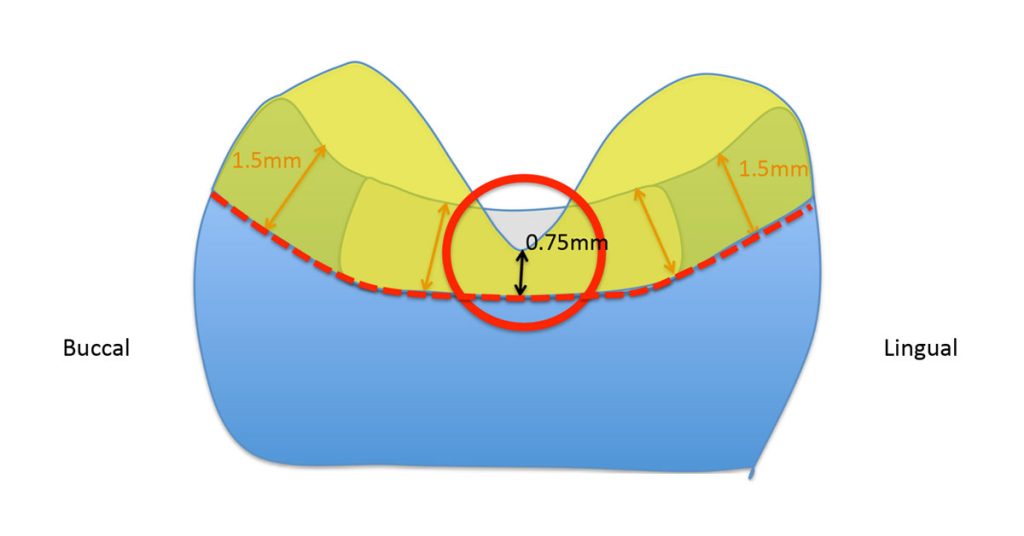
The bowl-shaped restoration was prepared to a 1.5 mm depth. Indeed, this is an adequate thickness for a ceramic bonded to dentin. However, no depth consideration was given to a change in the final restoration’s anatomy. Placing a final restoration with improved anatomy will create a potential for fracture and failure due to the inadequate thickness in the central groove of the occlusal surface.
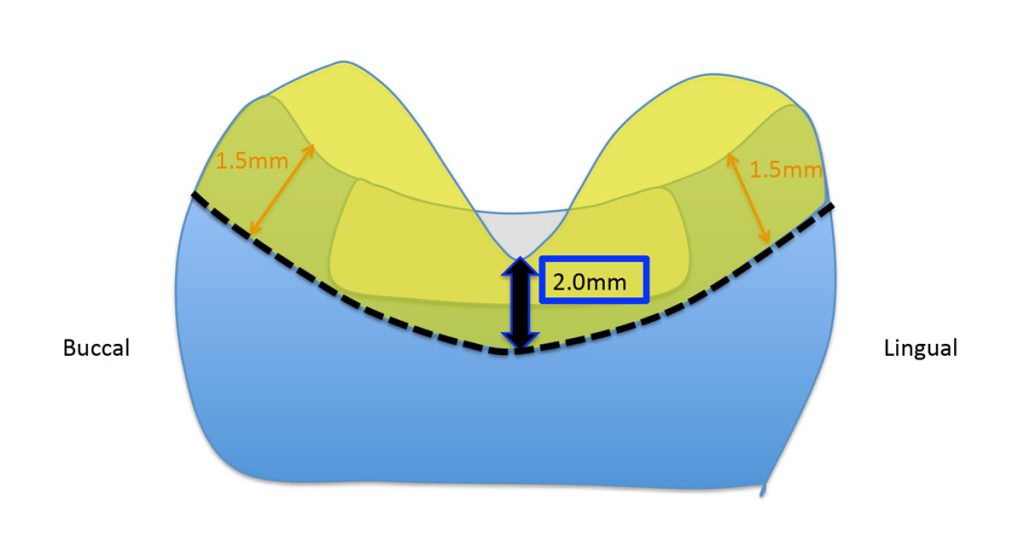
Diagram 4 shows that a greater reduction (2.0 mm) was utilized in the occlusal groove to compensate for the more ideal anatomy integrated into the final ceramic onlay. This preparation design factor improves the longevity of the partial coverage restoration.
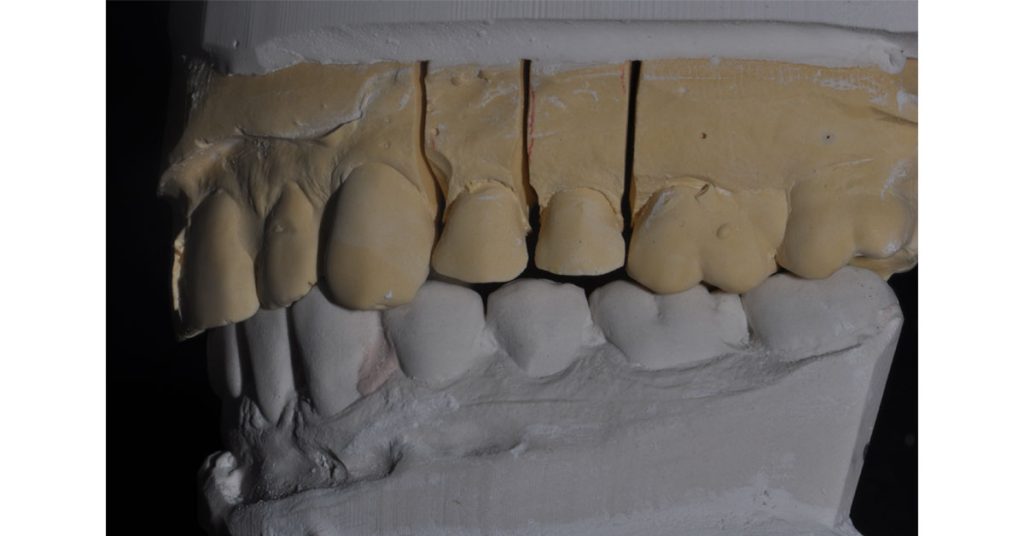
Long-term predictability may be achieved by incorporating proper planning and design into the posterior partial coverage ceramic restorations. This patient had significant erosion due to gastroesophageal reflux disease.
He had lost cuspal height and contour. The full-contour e.max ceramic onlays were fabricated with adequate thickness and ideal anatomy using the diagnostic wax-up as a guide for outcome-based tooth preparation. These restorations have now been functional for more than five years.
The following photos show the final ceramic onlays for the patient’s #12 and #13 teeth:
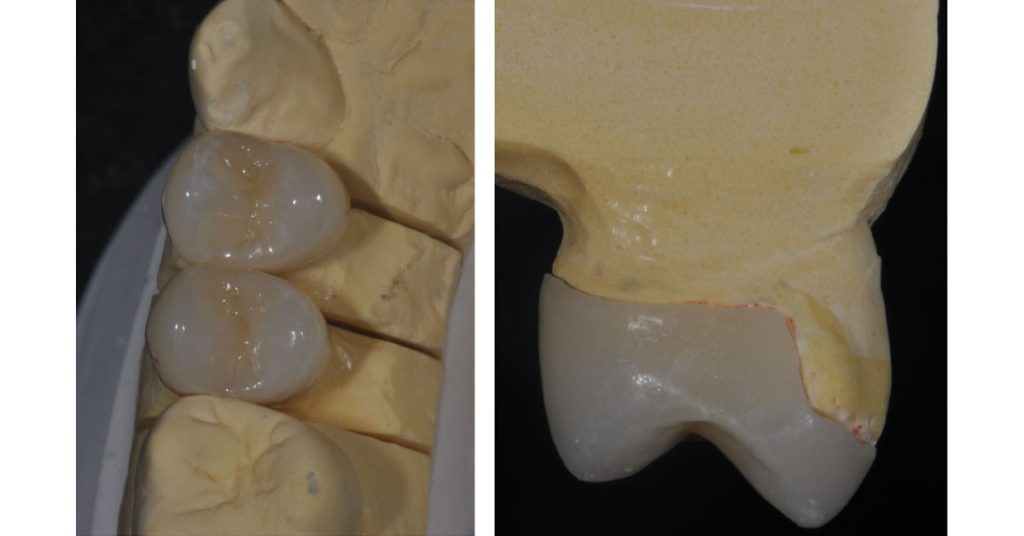

The “ideal reduction sauce” for these cases is to provide adequate space for anatomic contour and material strength. Proper planning and execution create predictable and long-lasting results.
Whether we are talking about ceramic onlays or great food, success stems from proper planning. The ideal “reduction” is all about the preparation!
SPEAR campus
Hands-On Learning in Spear Workshops
With enhanced safety and sterilization measures in place, the Spear Campus is now reopened for hands-on clinical CE workshops. As you consider a trip to Scottsdale, please visit our campus page for more details, including information on instructors, CE curricula and dates that will work for your schedule.

By: Jeffrey Bonk
Date: July 29, 2019
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


