- Occlusion / Wear
3 Key Clinical Steps for Successful Denture Insertion
The denture delivery appointment can be an exciting and highly anticipated day. Depending on the method of denture fabrication, the patient, dentist, and dental technician may have been working toward this day over the course of three to seven (or even more!) different clinical appointments and multiple trips in and out of the dental laboratory.
Despite all the care and precision that have gone into the case so far, from diagnosis and treatment planning through wax try-in, there is almost always some level of anxiety present. Wouldn’t it be great if we could simply hand the dentures to our patient and know that everything is perfect? No adjustment to the denture needed. No adaptation by the patient needed? Maybe someday …
(Click here to read nine steps to conventional complete denture fabrication.)
Until then, clinicians will need to carefully evaluate and adjust each new prosthesis to create the best chance for patient adaptation. As Kratochvil pointed out in 1966, “The insertion appointment is the process of eliminating errors.”
While the denture insertion appointment may seem fairly straightforward, there are several areas that clinicians will need to carefully evaluate to provide the most atraumatic prostheses possible. Let’s walk through the key steps involved with the denture insertion appointment.
Step 1: Adjust denture intaglio
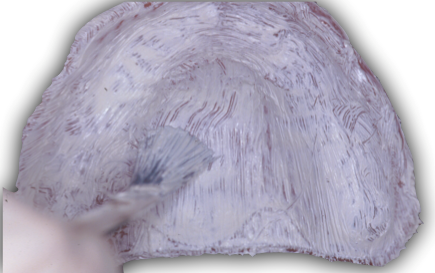
The first step involves making sure the denture has a stable relationship with the denture-bearing mucosa. Typically this evaluation and adjustment will be performed on one arch at a time, using a pressure-indicating medium.
Pressure-indicating paste is commercially available from Kerr and is convenient for clinicians who aren’t treating complete denture patients in high volume. As a lower-cost alternative, clinicians can make their own paste by mixing 50% lanolin with 50% zinc oxide powder. The custom-mixed paste may be stored in a disposable Monoject syringe until ready for use. In either case, this type of paste works best when applied to a dry denture surface.

Some authors have advocated using a silicone paste, for example GC’s Fit Checker. While effective, the effort required to mix by hand the multiple batches that would be necessary at a denture insertion appointment is cumbersome. Still, this could be a good option in a pinch.
Whichever paste is used, the indicating medium should be applied to the denture. The clinician then carefully inserts the denture, holding pressure in the area of the first molars. Common adjustments include areas with bony or soft tissue undercuts, the maxillary tuberosities, hauler notch, and retromylohyoid areas.
Step 2: Flange extension
Once the denture is seating well, the next step is to evaluate and adjust the denture flange areas. Overextended denture flanges may contribute to decreased denture stability and retention. Furthermore, if not fixed, overextended denture flanges may create ulcers in the vestibular sulcus.
(Click here to read considerations on dentures and patient’s quality of life.)
Visualizing the denture extension into the sulcus can be difficult clinically. Pressure-indicating paste, as described above, doesn’t work as well in evaluating the denture flange because it is wiped away so easily by the moveable mucosa, resulting in false positives. Disclosing Wax (Kerr) has been used with better success. These adjustments are, again, performed one arch at a time.
To use disclosing wax:
- Dry the denture border in the area being evaluated, place the wax, then carefully seat the denture.
- Once seated, hold the denture in place and have the patient move through border-molding movements. As the wax warms up, it will be accurately molded.
- Carefully remove the denture and inspect. Overextended borders will have had the wax removed. These areas should be marked and then removed with a carbide bur.

Recently Haeberle et al. have described a similar technique for identifying overextended denture flanges. Their technique is nearly identical to the one described above but rather than using wax, the authors used a fast -etting silicone bite registration material. The key benefit to using this material is the significantly easier cleanup.
Ultimately, any areas of the denture flange that have been adjusted must be smoothed and highly polished before the patient is allowed to leave with the new dentures.
Step 3: Occlusion
The final step in this sequence is evaluating the occlusion. Note that up until now, the dentures have been tried in individually and the denture teeth have not been allowed to contact their opposing counterparts. Ideally, occlusal evaluation and adjustment would be done with a clinical remount. This procedure will be described in greater detail in an additional article.


With or without a clinical remount, it’s best to evaluate the denture occlusion after the denture-bearing mucosa has had a chance to “settle.” Ask the patient to bite firmly onto cotton rolls placed over the first molars for 4–5 minutes. Next, remove the cotton rolls and have the patient slowly close. It’s not uncommon for the dentist to need to stabilize the lower dentures with some finger pressure at this point.
Conclusion
The completed prostheses are the culmination of care, skill, and judgment on the part of both the dentist and the dental technician. Despite really good technique, the completed prostheses are also the sum of all the inaccuracy introduced into the case. Following a repeatable sequence of steps at the insertion appointment improves efficiency for clinicians.
Setting realistic expectations is key for success with complete dentures. Patients should be informed and reminded that there will be a period of time required for adaptation to the new prostheses. Even the best denture will require some “getting used to.”
Typically the denture insertion appointment will be followed by a postinsertion appointment at 24 hours, one week, and again at one month. Each of these appointments will follow the same sequence of adjustments.
I hope you have found this information helpful. Look for follow-up articles in the future. You may consider sharing this sequence for the denture insertion appointment with your team to allow them to support the patient through the course of treatment.
References
- McCord JF, Grant AA. Prosthetics: Trial dentures, insertion of processed dentures and review of complete dentures. British Dental Journal 2000; 189:4-8.
- Yeoman LR, Beyak BL. Patient’s ability to localize adjustment sites on the mandibular denture. J Prosthet Dent. 1995; 73(6):542-547.
- Kivovics P, Jáhn M, Borbély J, Márton K. Frequency and location of traumatic ulcerations following placement of complete dentures. The International Journal of Prosthodontics 2007; 20(4):397-401.
- Bookhan V, Owen CP. A comparison of the cost effectiveness of pressure-indicating materials and their ability to detect pressure areas in complete dentures. SADJ. 2001; 56(5):228-232.
- Logan GI, Nimmo A. The use of disclosing wax to evaluate denture extensions. J Prosthet Dent. 1984; 51(2): 280-281.
- Haeberle CB, Abreu A, Metzler K. Use of a bite registration vinyl polysiloxane material to identify denture flange overextension and/or excessive border thickness in removable prosthodontics. Gen Dent 2015.
- Shigli K, Angadi GS, Hegde P. The effect of remount procedures on patient comfort for complete denture treatment. J Prosthet Dent. 2008; 99(1):66-72.
- Al-Quran FA. A clinical evaluation of the clinical re-mount procedure. J Contemp Dent Pract. 2005; 15(6): 48-55.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Darin Dichter
Date: April 16, 2018
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


