Pulp Capping: Can We and Should We?
Management and restoration of deep carious lesions can be a challenging dilemma faced in our daily practice. In a previous article, I briefly highlighted considerations when managing deep carious lesions. One of the considerations was whether or not to perform a pulp cap prior to restoring a tooth with a deep carious lesion.
Pulp capping can be divided into two categories: indirect pulp capping and direct pulp capping. For an indirect pulp cap, a carious lesion approaches the pulp tissue, but a pulp exposure does not occur. With a direct pulp cap, the pulpal tissue is exposed, and a medicament is placed over the exposure. Both procedures have historically been controversial. However, with a greater focus on conservative dentistry and more research on pulp capping, this topic is being discussed more frequently.
Can We Pulp Cap?
One of the significant controversies in the past with pulp capping questioned whether or not a pulp cap can be successful. For indirect pulp capping, the pulp tissue is never exposed, and as a result, this procedure tends to demonstrate higher success rates.
Indirect pulp capping can occur in either a one-step or two-step process. In the one-step process, a medicament is placed in the deepest aspect of the preparation, and the definitive restoration is immediately placed.
A provisional restoration is placed in the two-step procedure, and the tooth is re-accessed at a second visit. The theory behind a two-visit procedure is that the initial caries excavation and provisional restoration will help change the composition of bacteria in the tooth, making it less likely to expose the pulp during the second appointment. However, research has shown that the one-step procedure shows greater success than the two-step procedure.1




A direct pulp cap exposes a portion of the pulp tissue. This can occur due to traumatic or carious pulp exposures. In the past, when a tooth’s pulp was exposed, it almost always led to endodontic therapy. However, direct pulp capping may be feasible in specific clinical situations with modern materials that can help maintain pulp vitality, such as MTA and similar bioceramics.
Various studies have shown that direct pulp capping can be successful,2,3 and much of the research published on this topic in the endodontic community has shown that it can be a predictable procedure to maintain tooth vitality. This is even the case when a carious pulp exposure occurs in mature permanent teeth.4




Should We Pulp Cap?
Knowing that we can perform pulp capping predictably, it is important to determine if and when we should perform these procedures.
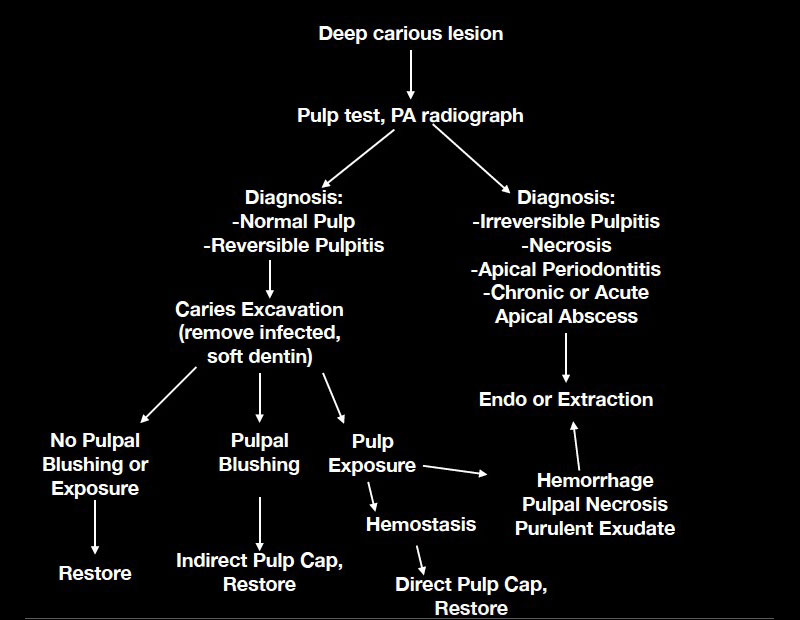
One key factor is to determine the endodontic diagnosis of a tooth with a deep carious lesion prior to starting treatment. Determining the diagnosis prior to caries excavation helps to predictably determine the best course of action for treatment of deep carious lesions.
Another key factor is isolation. In general, when a carious lesion is near the pulp chamber, it is advised to utilize rubber dam isolation. This helps minimize any contaminants in the preparation and simplifies the transition to endodontic therapy if pulp exposure occurs, which necessitates it.
Teeth with a normal pulpal response or a symptomatic reversible pulpitis response to cold stimuli have the potential to remain vital after pulp capping. However, upon cold testing, teeth that present with symptomatic irreversible pulpitis or pulpal necrosis are not candidates for pulp capping procedures. Furthermore, teeth with percussion or palpation sensitivity, or a radiolucency at the root apex, indicate the presence of apical periodontitis and are poor candidates for pulp capping.
The experience of “can we” and “should we” pulp cap came out of necessity in the clinic I previously worked in, where we routinely treated young adults with vital teeth with large carious lesions near the pulp. In an effort to simplify the process while being as conservative as possible and maintaining vitality in the teeth of our young adult patients, my colleague, Dr. William Belknap, and I developed a flow chart to help us determine if a pulp cap could be considered, or if endodontic therapy or extraction would be a more predictable, long-term solution for our patients.
In summary, the research shows that we can predictably perform pulp capping procedures using the bioceramic materials currently available.
The endodontic diagnosis determines whether or not we should consider pulp capping for our deep carious lesions. If we have a vital, normal pulp, our chances of successfully maintaining vitality are much greater. However, other treatment options should be considered if we have a symptomatic or necrotic tooth.
References
- Hoefler, V., Nagaoka, H., & Miller, C. S. (2016). Long-term survival and vitality outcomes of permanent teeth following deep caries treatment with step-wise and partial-caries-removal: a systematic review. Journal of Dentistry, 54, 25-32.
- Asgary, S., Hassanizadeh, R., Torabzadeh, H., & Eghbal, M. J. (2018). Treatment outcomes of 4 vital pulp therapies in mature molars. Journal of Endodontics, 44(4), 529-535.
- Hilton, T. J., Ferracane, J. L., Mancl, L., & Northwest Practice-based Research Collaborative in Evidence-based Dentistry (NWP). (2013). Comparison of CaOH with MTA for direct pulp capping: a PBRN randomized clinical trial. Journal of Dental Research, 92(7_suppl), S16-S22.
- Suhag, K., Duhan, J., Tewari, S., & Sangwan, P. (2019). Success of direct pulp capping using mineral trioxide aggregate and calcium hydroxide in mature permanent molars with pulps exposed during carious tissue removal: 1-year follow-up. Journal of Endodontics, 45(7), 840-847.
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Andy Janiga
Date: July 20, 2020
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


