- Beyond Restoration
4 Questions To Ask When Evaluating Cracked Teeth
What do you do or recommend when your patient has a cracked tooth? If you are like me, there’s no “one” answer because the answer depends on many factors.
In this article, I will outline some key factors to consider when evaluating your cases and trying to come to a solid recommendation for your patients that fits their particular situation.
1. Is the tooth painful to pressure?
If the answer is yes, the next question to ask is if the pain is upon biting and applying the pressure, or upon release. If it’s upon application of pressure, then I’m thinking it’s either an apical abscess or root fracture. The root fracture can often be confirmed by a periodical radiograph or by the presence of a deep isolated probing depth. An apical abscess would be confirmed via percussion sensitivity, a periapical radiograph, and/or a negative response to vitality testing. If, on the other hand, the pain is upon release, then I’m thinking along the lines of cracked tooth syndrome. For testing biting sensitivity, I most often use a tool called a Tooth Slooth.

This tool works by placing the pointed end on each cusp, as pictured below, then having the patient bite and release. A normal, healthy tooth will have no pain.

If the tooth is only suffering from cracked tooth syndrome, then a crown may be all it needs. For these teeth, I typically temporize them to see if the patient’s symptoms resolve, unless the patient has lingering pain to thermal testing and we know endodontic treatment is indicated.
Lastly, in the case of root fracture, the tooth is often a loss, although in some cases it can be kept via root amputation or hemisection. So at the end of the day, the short answer for these teeth is: It’s a safe bet to recommend placing a crown if the tooth is to be retained.
2. Where is the crack?
Is the crack only on the surface or is it internal? And if it is internal, is it under a cusp or right across the center of the pulpal floor?
For me, if it is in the enamel only, I consider it a craze only and not a true crack. Therefore, I would typically not recommend a crown. If, on the other hand, I can see the crack internally upon prep and it’s under a cusp, I get concerned that if the crack propagates after I restore the tooth with an intercoronal restoration, the cusp in question may fracture off. This would require a new restoration. Taking it further, if the crack is across the pulpal floor, then I worry more about catastrophic fracture propagation and possible loss of the tooth.
The next question for me when there is a crack I can see internally is, “What does the rest of the tooth look like?” If the tooth is pretty solid except for a fracture under one cusp, I would likely recommend that the cusp in question be covered by doing an onlay or 3/4 crown. However, if all the cusps are weak or I’m worried about a catastrophic failure of the tooth, I would recommend a crown.
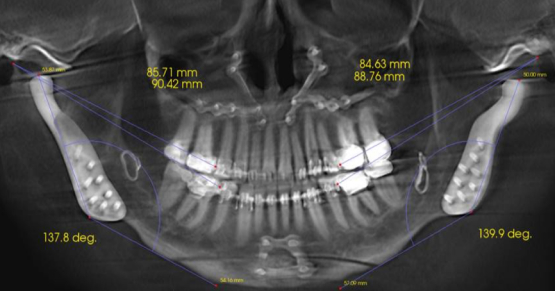
3. What is the patient’s occlusion like?
This plays a big role for me, because this may be the underlying cause of the crack. If their bite is not or has not been idealized to lessen the potential for further destruction, then I would highly consider doing this if the patient is agreeable. Along this line, a big thing to consider is if the tooth in question is the patient’s first point of contact in centric relation. Not only does this give a big clue as to why you are seeing the crack, you also could be in for big trouble if you just go do a crown on the tooth. For more on that, check out this previous Digest article on tooth preparation.
4. What is the patient’s risk tolerance?
This is perhaps the biggest factor and consideration. As hard as it is to accept, we sometimes want more and/or better for our patients then they do! For example, take the scenario mentioned above of a crack under a cusp. If we did an intercoronal restoration, that cusp with the fracture under it might come off later, at which time a new restoration would be needed. While we might view having to do a new restoration as a big deal, our patient may not. If they don’t view that as a big deal, then they may elect to just do an intercoronal restoration.
Going even further, the patient may be OK with way more severe consequences, such as even losing a tooth. In my practice I am fine with this, assuming they are truly OK with the potential consequences and I’m sure they’re really OK with them (not just saying they are as an easy out). The thing you have to be careful about here is that the patients have to understand and be OK with the full impact of the potential consequences for not only the tooth in question, but also their other teeth, overall health, and stated goals.
To bring this thought process into play on an actual case, let’s look at a case I had in my office. Preoperatively, the lower second molar had a relatively small failing alloy and looked to have a craze line over the mesial marginal ridge, as noted in the photo below.
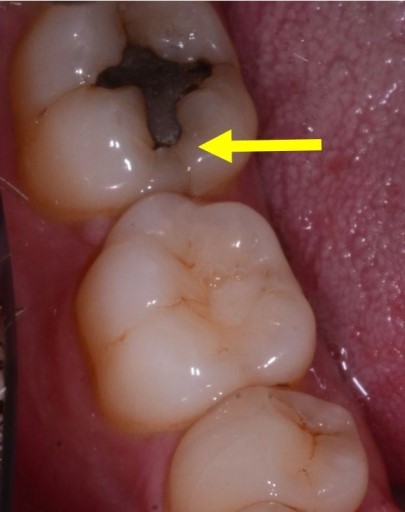
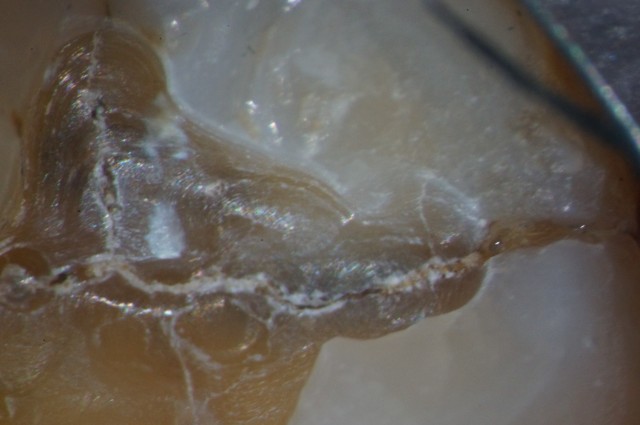
There was also a more suspicious possible fracture, pictured below.

Our plan and hope was to replace the failing alloy with a new composite, assuming of course we found no fracture inside the tooth. Unfortunately, upon preparation, here is what we found.

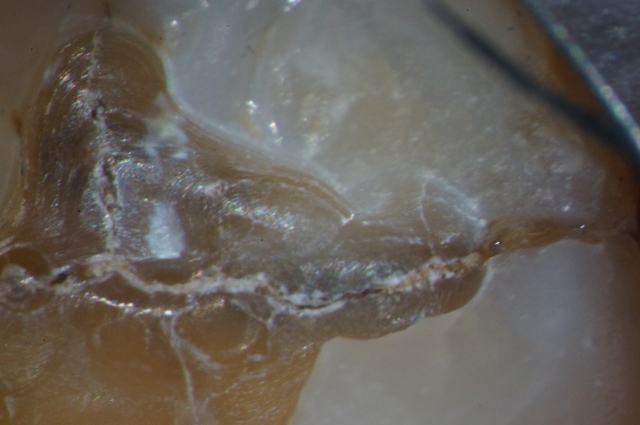
As you can see, there were multiple fractures inside this tooth. To add to the concern, this tooth is also the patient’s first point of contact in centric relation.
Because of the discovery of clear internal fractures as well as the fact that this was the patient’s first point of contact, I recommended placing a composite as a core build-up. Then we’d place a crown as the final restoration after working the patient’s occlusion out, so we wouldn’t end up in trouble after preparing the tooth for a crown, as discussed in this article on why temporaries keep coming off.
That’s what I recommended, based upon the patient’s occlusion and condition of the tooth. But what we ended up doing, based on the patient’s risk tolerance, was an occlusal composite only!
VIRTUAL SEMINARS
The Campus CE Experience
– Online, Anywhere
Spear Virtual Seminars give you versatility to refine your clinical skills following the same lessons that you would at the Spear Campus in Scottsdale — but from anywhere, as a safe online alternative to large-attendance campus events. Ask an advisor how your practice can take advantage of this new CE option.

By: John Carson
Date: June 29, 2016
Featured Digest articles
Insights and advice from Spear Faculty and industry experts