Using the Matrix Technique for Repairing Debonded Denture Teeth
Despite recent interest in digitally designed and manufactured dentures, today most conventional complete dentures are traditionally fabricated and predominantly made up of acrylic resin, a material that doesn’t hold up well to impact (i.e., drops) or fatigue.
As a result, it should be expected that the prosthesis will not last forever, partly due to material breakdown. This breakdown may appear clinically as denture base fracture, denture tooth wear, and/or denture tooth fracture (Fig. 1).

A metal framework is frequently used when implants are introduced into an edentulous case (Fig. 2).

The use of a metal introduces an interface, the acrylic/metal interface, that can fail as the prosthesis ages. Additionally, implants will significantly increase the magnitude of force applied to the materials, often hastening materials breakdown when compared to conventional complete dentures.
Unfortunately, time under function is not the only enemy of acrylic or metal-acrylic prostheses. Material failure can occur if the prosthesis is dropped or the patient is involved in a traumatic accident, for example. Fabrication error may also contribute to problems, particularly at the denture tooth/denture base interface, where residual wax contamination may inhibit an effective bond. Fortunately, despite its disadvantages as a biomaterial, acrylic resin is relatively easy to repair.
Clinical Scenario
The patient in Figure 3 was seen with the chief complaint of a debonded maxillary denture tooth and was concerned about the loss relative to his appearance.

The current reconstruction was completed by the patient’s previous restorative dentist just before the 2008 global financial crisis. It consists of a maxillary implant overdenture and a mandibular metal and acrylic fixed hybrid (Figs. 2 and 4).
When a denture tooth is separated or debonded from the denture base, understanding why is critical to the prognosis. In this patient’s case, the denture tooth appears to have been lost due to functional issues rather than a fabrication issue, like wax contamination. Based on this finding, a comprehensive evaluation was recommended for the patient.
In this case, at the time the patient was seen, he was financially unable to address comprehensive concerns and asked if the missing denture tooth could be repaired and the case limped along a little longer.

One advantage of a removable prosthesis is that it is easier to remove and modify or repair than a fixed prosthesis, even when the restorative materials are the same, as they are in this case. Based on the patient’s current circumstances, it was agreed that the maxillary overdenture would be repaired (Fig. 5).

Options
Several options exist to repair the debonded denture tooth. The most common and strongest approach would be to return the denture to a lab and have a new denture tooth positioned utilizing heat-processed acrylic resin. While common, this approach has two distinct disadvantages: the first is lab cost, and the second is time.
If the case goes to a lab, the new denture tooth will have a stronger bond to the denture base, but the patient will be without the denture while the repair is being made and will need to be seen for an additional clinical appointment for insertion.
A second option would be freehand a new tooth utilizing restorative composite or even tooth-colored acrylic resin. While this may work in a pinch, to achieve a reasonable esthetic outcome most clinicians will find they spend significantly more time making this type of a repair compared to the next option.
The third option is to replace the missing denture tooth. The approach used here is to utilize a new, stock denture tooth and connect the tooth to the denture base with cold-cure (autopolymerizing) repair resin. This approach is made easier if the patient has retained the debonded tooth. In this case, the tooth was not recovered. The most significant disadvantage to this approach is that clinicians would need access to a selection of denture teeth.
Step 1: Select Replacement Tooth
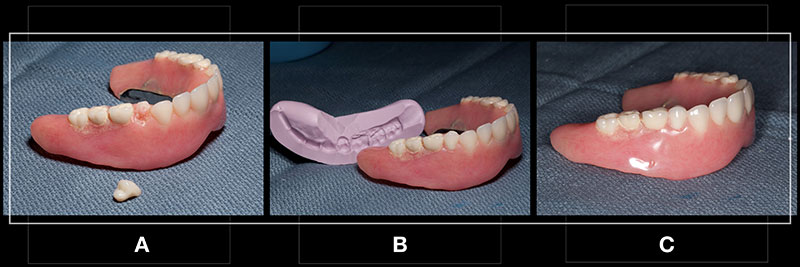
If the existing denture tooth is available — such as in a debond that resulted from wax contamination at the tooth/denture base interface — it may be possible and even preferable to re-use that tooth. In other situations, finding a new denture tooth may be necessary based on a similar tooth shade and tooth mould. The advantage of using the existing tooth is a reduction in the time required to fit a new tooth to the denture base (Fig. 6A).
Step 2: Fit Replacement Tooth to Existing Denture Base
Once the new denture tooth has been selected, it must be adjusted to fit into the base socket. Patience pays off with careful adjustments. In a 2014 paper, Auclair and Hsu found that as the repair resin increased, the bond strength between the denture tooth and base decreased.
Step 3: Fabricate Matrix
Once the new tooth has been adjusted to fit into the arch and socket, a matrix can be formed to ensure the denture tooth is positioned accurately during the repair. Traditionally, the matrix was made from plaster or stone, but it is common to use lab silicone putty (Fig. 6B).
Step 4: Prepare Surfaces for Repair
Many researchers have looked at approaches to maximizing the bond of the denture tooth to the denture base during this kind of repair. The research is clear that the repaired tooth will have a weaker bond to the denture base than the original situation. The bond strength can be maximized, however, by mechanically roughening the surfaces to be bonded with a carbide bur and micro air abrasion, as well as utilizing undercuts or diatorics.
Step 5: Connect Denture Tooth to Denture Base
Once the tooth and the denture base are prepared it is just a matter of making the connection. Denture repair acrylic resin is inexpensive and is designed for this type of operation, but a self-curing bisacryl luting material, like Quick-Up (Voco GmbH), could also be used.
Step 6 : Finish and Polish
The degree of finishing required will relate to the precision of fit of the denture tooth to the denture base and the amount of repair material required. Yet, even in the worst case, the step should be pretty efficient (Fig. 6C).
Occlusal Considerations
The final challenge with this technique is managing the occlusion. In this case, the replacement tooth was positioned within the arch form and “eye-balled” to be level with the existing occlusal plane. This approach required the occlusion tobe adjusted clinically, which is like adjusting a single crown. These adjustments could have been minimized by articulating the upper denture with a clinical remount against a stone cast of the opposing arch — not a bad idea if other occlusal issues are going to be managed.
The primary advantage of this technique is efficiency in chair time. In this case, the repair was made in just under 60 minutes during a single appointment and could have easily been done by a trained staff member. The disadvantage is it is impossible without having at least a small supply of denture teeth available. The biggest technical difficulty is making the adjustment to the denture tooth to get the neck of the tooth to fit to the denture base.
References
- Barpal, D., Curtis, D. A., Finzen, F., Perry, J., & Gansky, S. A. (1998). Failure load of acrylic resin denture teeth bonded to high impact acrylic resins. The Journal of Prosthetic Dentistry, 80(6), 666-671.
- Chung, K. H., Chung, C. Y., Chung, C. Y., & Chan, D. C. N. (2008). Effect of pre‐processing surface treatments of acrylic teeth on bonding to the denture base. Journal of Oral Rehabilitation, 35(4), 268-275.
- Clark, W. A., & Hsu, Y. T. (2014). The effect of autopolymerizing acrylic resin thickness on the bond strength of a repaired denture tooth. Journal of Prosthodontics, 23(7), 528-533.
- Boucher, C. O., Hickey, J. C., Zarb, G. A., & Swenson, M. G. (1975). Prosthodontic treatment for edentulous patients. (No Title).
SPEAR ONLINE
Team Training to Empower Every Role
Spear Online encourages team alignment with role-specific CE video lessons and other resources that enable office managers, assistants and everyone in your practice to understand how they contribute to better patient care.

By: Darin Dichter
Date: August 5, 2020
Featured Digest articles
Insights and advice from Spear Faculty and industry experts


