Managing Oligodontia: A Case Report
Oligodontia is a hereditary disorder characterized by the agenesis of six or more teeth. It’s a dental abnormality in patients with multiple missing teeth.

The teeth that are most often absent are the premolars (15 to 32%), the maxillary lateral incisors (27%), and the third molars (25%). Rarely are the canines, central incisors, and the first molars absent. It is common to see the existing teeth undersized or conical in shape. There are retained primary teeth and often delayed eruption of permanent teeth.
Oligodontia is associated with various genetic syndromes, including ectodermal dysplasia, Van Der Woude syndrome, and Down syndrome. Alternatively, it occurs as a non-syndromic isolated familial trait. Differentiation between syndromic and non-syndromic forms is determined from physical examination of the hair, nails, sweat glands, and eyes to evaluate a genetic disorder.
Once the diagnosis has been determined, managing the multiple missing teeth is necessary. The patient’s difficulties include mastication, altered occlusion, affected speech, and altered facial appearance that affects the patient’s esthetics and psychology.
The treatment of oligodontia is complex and lengthy. Management of these cases begins around the age of eight. Because of this young age, the treatment process must be phased over several years due to growth and development. It typically involves multiple dental specialties (orthodontics, periodontics, oral surgery, and prosthodontics) to provide definitive treatment. Treatment planning for these complex cases must include the Spear FGTP concepts. The goal is to help direct the interdisciplinary team and provide guidance and reassurance to the patient and family that the restoration will lead to a normal life.
Oligodontia Treatment for Teenage Patient
This case report is reviewed to best outline the management of a single oligodontia case. My orthodontic colleague and team member referred Jessica to my practice. She was 14 years old at the time of my initial examination.

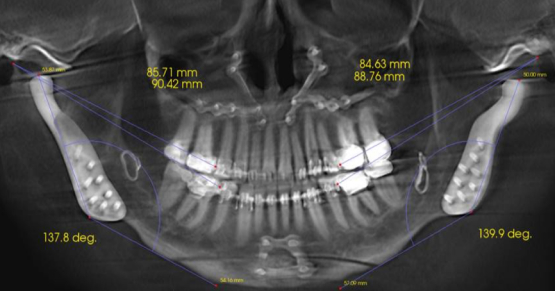
Before my exam, the orthodontist treated and consolidated Jessica’s existing permanent teeth. He created tooth spaces for restoring missing permanent teeth and used fixed wires to maintain tooth position. The long-term treatment goal was to utilize implant-supported restorations when growth and development had finished.
Jessica’s primary concern was that “she wished she could change the appearance of her smile.” As discussed earlier, the esthetic effects of multiple missing teeth are a significant factor in these patients with oligodontia. Jessica was not comfortable with her tooth spaces and her small and worn retained primary lower teeth.
Although her prosthodontist had provided a “flipper” to replace the missing upper lateral incisors, she could not masticate or function well. She desired some “permanent” tooth replacements. She presented with no medical issues that would prevent dental restoration. Hers was a non-syndromic form of oligodontia. Her family (mother) did have a history of missing permanent teeth, but no one as severe as hers.
To provide Jessica with a “permanent” tooth replacement until she was old enough for implant therapy, I needed to plan the treatment for the tooth size and positions that would act as replacements. The goal is to provide esthetics, comfort, and function so she can become a “normal” adolescent and “fit in” with her peers.
Creating the Diagnostic Wax-Up
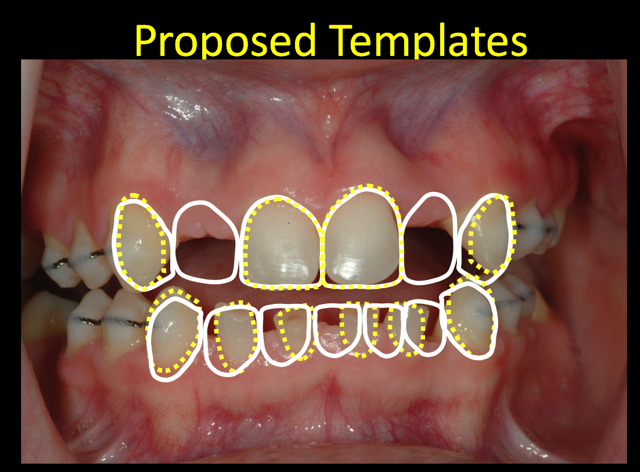
I applied the FGTP concepts taught in the Spear curriculum to establish tooth size and position. As you observe from the image provided, the remaining permanent teeth had tooth size discrepancies.
The microdontia that commonly occurs with oligodontia requires restoration of tooth size. The maxillary cuspids require increased contouring to improve esthetics and provide more normal-sized lateral incisors.
It is common with oligodontia to have retained primary teeth. Without the permanent tooth replacements, the primary tooth roots do not resorb at the expected rate. The templates provide opportunity to preview possibilities for tooth size and shape changes.
For the lower anterior teeth, an additional incisor can improve esthetics. The template proposal was presented to Jessica and her parents. The esthetic corrections were pleasing to everyone. Models and bite recordings were obtained to create a diagnostic wax-up to determine function and evaluate restoration possibilities.
The diagnostic wax-up was completed. The wax-up allows proposed template changes to be applied directly to the tooth model. This wax-up was both reductive and additive. In the lower anterior region, the primary teeth were reduced in dimension to allow for the wax addition of an extra incisor. The upper canines were enlarged to a more normal size. The molar regions were filled in to complete the process.
Because the models were mounted on articulators, the functional aspects could be evaluated. The wax-up provides the “blueprint form for clinical restorative changes.”
Final Steps in Oligodontia Treatment
The final treatment plan was outlined for Jessica and her parents. Resin-bonded bridges would be utilized as the interim restoration of choice to provide esthetics and function until the implant phase could be initiated. The additive tooth dimension changes would be duplicated from the wax-up, using silicone templates as guides. The silicone indices would act as preparation guides for primary tooth reduction before the bonded bridges are placed.
The resin-bonded bridges were pre-made from duplicate wax-up models. Ribbond was incorporated into the lingual wings of the upper and lower anterior bridges. Glass-span ropes were utilized for structural support in the posterior bridges.

The upper posterior resin bridges were adhered to the abutment teeth. Jessica elected not to have the lower bridge fabricated to save expense. Following composite additions to the maxillary cuspids, the lateral incisor resin bridges were secured with flowable composite.
Once the lower anterior primary teeth were prepared, the lower bridge was tried in and adjusted for esthetics and function. It was luted with flowable composite to the remaining enamel.
The functional movements were adjusted and Jessica was released from our practice until she reached an age for implant therapy. She returned to her local dentist for routine dental hygiene care.
Five years later, Jessica returned to our office to pursue implant treatment. We reviewed her situation and planned for implant placement in the upper and lower posterior segments.
Jessica’s parents wished to stage the implant process and elected to begin in the posterior. The oral surgeon placed the implants, and once healed, screw-retained implant restorations were inserted. The post-treatment images show the molar implants in place. Additionally, seen in the photos are the upper and lower anterior provisional bridges. They remain intact from the original placement date.
Jessica has had no issues or problems with these provisional restorations. Other than some subtle changes in shade, they are expected to remain in place until Jessica is ready to pursue further implant treatment. It has already been more than two years since she had her molar implants restored, and it has been almost eight years since the provisional resin bridges were initially placed.
Fortunately, oligodontia is a rare finding. Hypodontia (less than six missing teeth) is more common. Having a significant number of missing teeth is challenging for the patients, relative to function and esthetics.
It is also challenging for dentists to manage these cases for an extended time. Hopefully, this case and discussion may provide insight and guidance for other Spear dentists who may encounter these cases in their practice.
References
- Arte, S., & Pirinen, S. Hypodontia. Orphanet Encyclopedia. 2004: 1–7.
- Tangade, P., & Batra, M. (2012). Non syndromic oligodontia: Case report. Ethiopian Journal of Health Sciences, 22(3).
- Hosur, M. B., Puranik, R. S., & Vanaki, S. S. (2012). Oligodontia: A case report and review of literature. World Journal of Dentistry, 2(3), 259-262.
SPEAR STUDY CLUB
Join a Club and Unite with
Like-Minded Peers
In virtual meetings or in-person, Study Club encourages collaboration on exclusive, real-world cases supported by curriculum from the industry leader in dental CE. Find the club closest to you today!

By: Jeffrey Bonk
Date: June 7, 2017
Featured Digest articles
Insights and advice from Spear Faculty and industry experts